Published online Mar 28, 2015. doi: 10.3748/wjg.v21.i12.3663
Peer-review started: September 10, 2014
First decision: November 14, 2014
Revised: December 24, 2014
Accepted: January 21, 2015
Article in press: January 21, 2015
Published online: March 28, 2015
AIM: To examine the frequency of regular complementary and alternative therapy (CAM) use in three Australian cohorts of contrasting care setting and geography, and identify independent attitudinal and psychological predictors of CAM use across all cohorts.
METHODS: A cross sectional questionnaire was administered to inflammatory bowel disease (IBD) patients in 3 separate cohorts which differed by geographical region and care setting. Demographics and frequency of regular CAM use were assessed, along with attitudes towards IBD medication and psychological parameters such as anxiety, depression, personality traits and quality of life (QOL), and compared across cohorts. Independent attitudinal and psychological predictors of CAM use were determined using binary logistic regression analysis.
RESULTS: In 473 respondents (mean age 50.3 years, 60.2% female) regular CAM use was reported by 45.4%, and did not vary between cohorts. Only 54.1% of users disclosed CAM use to their doctor. Independent predictors of CAM use which confirm those reported previously were: covert conventional medication dose reduction (P < 0.001), seeking psychological treatment (P < 0.001), adverse effects of conventional medication (P = 0.043), and higher QOL (P < 0.001). Newly identified predictors were CAM use by family or friends (P < 0.001), dissatisfaction with patient-doctor communication (P < 0.001), and lower depression scores (P < 0.001).
CONCLUSION: In addition to previously identified predictors of CAM use, these data show that physician attention to communication and the patient-doctor relationship is important as these factors influence CAM use. Patient reluctance to discuss CAM with physicians may promote greater reliance on social contacts to influence CAM decisions.
Core tip: Complementary medicine use is widespread in inflammatory bowel disease, and potentially deleterious to treatment outcomes. Whilst demographic and clinical predictors of complementary and alternative therapy (CAM) are well established, attitudinal influences are under explored. This study demonstrates that the specific aspect of patient doctor relationship most influencing CAM use is quality of doctor communication. The other newly identified predictor of CAM use is its use by family and friends. This finding enables valuable insight suggesting that in the absence of good doctor communication, inflammatory bowel disease patients seek advice from unqualified sources such as family and friends.
- Citation: Mountifield R, Andrews JM, Mikocka-Walus A, Bampton P. Doctor communication quality and Friends' attitudes influence complementary medicine use in inflammatory bowel disease. World J Gastroenterol 2015; 21(12): 3663-3670
- URL: https://www.wjgnet.com/1007-9327/full/v21/i12/3663.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i12.3663
The use of complementary and alternative medicine (CAM) is widespread in inflammatory bowel disease (IBD), rates ranging from 31% to 74% in studies across Europe[1-3], Australasia[4,5], and North America[6]. Studies examining the efficacy and safety of these treatments in IBD are heterogenous and controlled data limited[7], thus it is difficult for physicians to advise patients regarding these potentially deleterious agents. However, the ongoing consumer demand for alternatives to conventional therapy means that IBD physicians need to be alert to CAM use, its associated behaviours and underlying health beliefs that may influence conventional IBD care.
Approximately three quarters of CAM taking IBD patients do not discuss its use with their IBD physician[3,8], thus there is a need to identify surrogate markers or predictors of use that may prompt discussion about CAM during routine consultation.
Predictors previously established fall into demographic, clinical and attitudinal categories. Independent demographic predictors of CAM use include younger age[1,5,9], female gender[1,5,9], higher educational level[5,9], income and employment[5,8], and middle social class at birth[5]. Clinical predictors are more controversial[10,11] but have included Crohn’s disease[9], longer disease duration[12], medication type[1,13], active disease[14], the experience of adverse effects of conventional medication[2,14,15], and a concurrent diagnosis of irritable bowel syndrome (IBS)[16].
Some studies however, have suggested that health attitudes and behaviours are more important than demographics in influencing CAM use[15,17], and there has been recent enthusiasm to identify attitudinal and behavioural predictors as these factors are potentially modifiable. Data regarding such predictors are more limited and heterogenous but suggest that a need for control over disease[17], desire for a holistic approach[17], lack of confidence in the IBD physician[17], poorer therapeutic relationships[18], and vegetarianism[5] are associated with CAM use. CAM use has also been suggested as a marker of psychological or social distress[16].
Disparity in findings between different studies may relate in part to cultural differences in IBD populations, as suggested by an Italian study which demonstrated regional variations in CAM type chosen, despite similar rates of use across the cohorts[14]. An Australian diabetes study suggested an effect of health care setting on CAM use frequency, reporting private health insurance as an independent predictor of CAM use[19]. In IBD patients in Australia, whilst overall frequency and potential ethnically based differences in CAM use have been previously examined[4], attitudinal and psychological predictors of its use are unexplored, as is the effect of the health care setting on CAM uptake.
IBD patients from three different care settings in two distinct geographical locations in Australia were invited to participate. This method has been reported previously[20].
The first cohort came from a metropolitan public teaching hospital based specialist IBD Service at Flinders Medical Centre (FMC). This is a large, government funded hospital, offering secondary/tertiary care for a local regional population of 341000 with a Gastroenterology inpatient and outpatient service, and IBD nurses available to patients within working hours.
The second cohort consisted of IBD patients in an overlapping area, receiving their care via a metropolitan Private Practice setting. These patients were under the care of one of four male general Gastroenterologists with extensive experience in managing IBD, without attachment to a specialist IBD unit, or access to IBD specialist nurse support.
The third cohort consisted of IBD patients cared for via Royal Darwin Hospital (RDH), a public hospital in a very remote location in Northern Australia. When this study was conducted, IBD care in Darwin was undertaken predominantly by general practitioners (GPs) and general surgeons, with no specialist gastroenterologist residing in Darwin, and no IBD nurse. The nearest tertiary hospital is in Adelaide, SA, more than 3000 kilometres away.
Potential subjects were identified from IBD databases/hospital records in each location and mailed a questionnaire. Reminder letters were sent to non-responders after one and three months.
The opening section of the questionnaire sought demographic details including age, gender, disease type, indigenous, relationship and employment status as well as current or previous history of smoking.
In the following sections, A-D, participants answered questions assessing: (1) views regarding conventional IBD medications; (2) views regarding CAM; (3) quality of Life; and (4) psychological and personality traits. Where possible, validated instruments were used as described below.
IBD-specific CAM use was assessed by asking subjects to rate the frequency with which they use complementary or alternative medicine to treat IBD on an ordinal Likert scale. A dichotomous variable was then generated whereby “yes” responses encompassed those describing their use as “often” or “very often”, and “no” included responses “sometimes”, “rarely” and “never”.
Medication Adherence was assessed using the Morisky 4 item Self Report Measure of Medication Taking Behaviour[21,22], examining predominantly dose omission, and covert dose reduction (CDR), the tendency to take less than prescribed of IBD medication without prescriber awareness was assessed as a dichotomous variable (yes/no) based on answer to the question “I take less than prescribed of my IBD medication without telling my doctor”. This has been previously reported[20].
Free text responses regarding attitudes towards IBD medication and dose modification were encouraged.
Other non-standardised attitudinal statements were put to subjects, seeking their views regarding IBD treatment beliefs and attitudes. Some Likert data were collapsed into categories “yes” and “no” for data presentation, but analysed as ordinal data or continuous data using factor scores for regression analysis.
Anxiety and Depression were measured using the Hospital Anxiety and Depression Scale[23], higher scores indicating higher levels of anxiety or depression. Quality of Life was measured using the reliable and valid Short Inflammatory Bowel Disease Questionnaire[24].
The Spielberger State-Trait Personality Inventory[25-27] was used to assess and compare depressive symptoms, anxiety, anger and curiosity between cohorts in both the immediate (state) and long term (trait or personality characteristic).
Comparisons between cohort means and medians were performed using the Kriskal Wallis test for non-normally distributed values, and two tailed t test or ANOVA for normally distributed values. Pearson’s χ2 or Fisher’s exact test were applied as appropriate for categorical data.
Significant or trend associations at univariate level (P < 0.10) determined which variables were included in regression analyses, along with demographic factors.
Additional continuous variables summarising themes across the questionnaire were generated using principal component analysis for ordinal data using M Plus software (V5.2), for the purpose of data reduction. An oblique (oblimin) rotation was used of 37 of the 55 Likert scale items assessing all aspects of IBD treatment. An examination of the Kaiser-Meyer Olkin measure of sampling adequacy suggested the sample was favourable (KMO = 0.618). When loadings less than 0.4 were excluded, the analysis yielded an 8 factor solution. Scores for each of these 8 factors were normally distributed.
Binary logistic regression was used to assess predictors of CAM use as a dichotomous dependent variable, adjusting for age, gender, employment and relationship status.
A P value of < 0.05 was considered statistically significant. Apart from factor analysis, statistical calculations were performed using IBM SPSS Statistics for Windows, version 22, 2013 (IBM Corp). The statistical methods for this study were reviewed by Dr Reme Mountifield of Flinders Medical Centre, South Australia.
Response rates to the survey differed between cohorts, with 337/612 (55.1%) of FMC and 91/180 (50.5%) of SA private invitees participating, compared with 35/100 (35%) in Darwin (P < 0.0001). Non respondents did not differ from respondents by gender (P = 0.2), but there was a trend toward non respondents being younger than respondents (mean age 43.7 vs 50.3 years, P = 0.065) Darwin subjects were more likely be current or previous smokers, and to receive a disability support pension. This population has been previously reported[20]. Demographic data are summarised in Table 1.
| FMC (n = 337) | Private (n = 91) | Darwin (n = 35) | P value | |
| Mean age respondents (yr) | 50.3 | 52.2 | 48.4 | 0.35 |
| Mean age non respondents (yr) | 43.0 | 48.1 | 39.9 | 0.20 |
| Female respondents | 60.2% | 60.4% | 60% | 0.99 |
| Female non respondents | 55.7% | 52.4% | 40.7% | 0.07 |
| Crohn’s disease | 55.2% | 57.1% | 48.6% | 0.70 |
| Indigenous subjects | 0.9% | 1.1% | 2.9% | 0.37 |
| Current smokers | 11.1% | 13.6% | 17.1% | 0.09 |
| Previous smokers | 25.8% | 25.0% | 42.9% | 0.09 |
| Receiving disability support pension | 1.8% | 1.1% | 5.7% | 0.006 |
| Employed | 58.7% | 56.7% | 62.9% | 0.19 |
| Currently partnered | 92.2 | 95.3 | 93.3 | 0.61 |
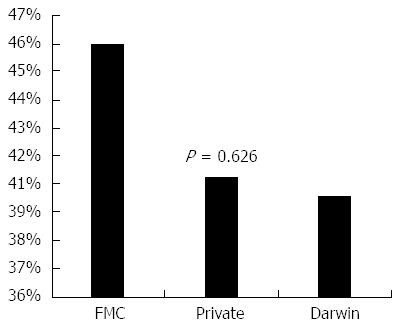
Many subjects (45.4% overall) reported regular use of CAM, with no significant difference in usage frequency between cohorts (P = 0.594) (Figure 1). Distribution of CAM type used is presented in Table 2, and was not significantly different between cohorts (P = 0.626). The regular use of more than one CAM type (i.e., physical as well as homeopathic methods) was reported by 64.5% of subjects.
| Primary (first mentioned) CAM type | Percentage of total CAM reported overall |
| Herbal products (e.g., slippery elm, aloe vera juice, olive oil extract, green lipped mussel oil, other herbs) | 30.50% |
| Probiotics | 22.60% |
| Fish oil | 12.10% |
| Chinese medicine | 10.50% |
| Acupuncture, massage, magnetism | 10.50% |
| Other (prayer, meditation, exercise, dietary supplements, hypnotherapy) | 13.70% |
Rates of CAM use were higher amongst younger (46.69 vs 53.41 years, P < 0.001), female (52.0% vs 35.5%, P < 0.001), and permanently employed (51.1% vs 37.4%, P = 0.004) subjects. However, CAM usage did not differ by disease type (P = 0.394), conventional medication pill burden (P = 0.784), smoking status (P = 0.805), or vegetarianism (P = 0.256) on univariate analysis.
Of the 206 subjects who reported regular CAM use, 52.5% felt that it was effective (worked “well” or “very well”), and 20.7% had obtained the therapy at consultation with an alternative practitioner rather than independently. The vast majority (83.3%) continued to use conventional IBD medications concurrently. Only half (54.1%) discussed their CAM treatment with their doctor, despite 87.6% of subjects reporting feeling comfortable doing so.
In contrast, of those reporting previous consultation with an alternative practitioner only 62.2% felt comfortable discussing conventional therapy with their alternative practitioner (P < 0.001), and 16.6% reported the CAM practitioner discouraged their use of conventional IBD medication. With regard to the consultation experience, 10.5% felt less intimidated by alternative practitioners than doctors, and 16.9% felt more informed about IBD by the alternative practitioner.
Of the 194/206 (94.2%) subjects who offered reasons for their CAM use, 33.0% reported safety concerns regarding conventional medications. Subjects who elaborated further expressed the belief that “natural” CAM would enable them to reduce reliance on “chemical” conventional therapy and dose reduce or cease these medications. Seeking a holistic approach to health in some way was cited by 32.0%, and 20.6% report advice from family, friends, colleagues, religious advisors, or the internet as their main reason for use. A smaller proportion (14.4%) cited lack of efficacy of conventional medications in treating IBD. No significant cohort based differences were observed.
Attitudinal and behavioural associations of CAM use on univariate analysis are presented in Table 3.
| Regular CAM use | P value | |||
| No | Yes | |||
| Deliberate dose reduction | No | 197 (61.4) | 124 (38.6) | < 0.001 |
| Yes | 46 (38.7) | 73 (61.3) | ||
| Family or friends use alternative treatments | No | 88 (55.0) | 72 (45.0) | 0.004 |
| Yes | 85 (40.1) | 127 (59.9) | ||
| Experienced adverse effects conventional IBD meds | No | 89 (59.7) | 60 (40.3) | 0.025 |
| Yes | 129 (48.3) | 138 (51.7) | ||
| Satisfied with communication with IBD doctor | No | 1 (9.1) | 10 (90.9) | 0.002 |
| Yes | 246 (55.7) | 196 (44.3) | ||
| Previous psychological counselling | No | 197 (61.6) | 123 (38.4) | < 0.001 |
| Yes | 49 (38.0) | 80 (62.0) | ||
Of all subjects including CAM users and non-users, 57.3% reported family or friends using CAM for any health purpose. Those with CAM-using contacts was more likely to use it themselves for IBD (59.9% vs 40.1%, P = 0.004), free text responses suggesting that type of CAM chosen was influenced by social contacts.
The 54.9% of subjects reporting adverse effects of conventional medications were more likely to use CAM (P = 0.025), as were the 26.9% reporting regular self-initiated dose reduction of medication (P < 0.001). Lack of doctor communication satisfaction was reported by only a small proportion of patients (2.4%) but was associated with CAM use, as was seeking of psychological or psychiatric treatment (P < 0.001) when analysed as individual items.
Analysis of HADS, QOL and Spielberger mean scores suggested that increased anxiety, higher quality of life and lower depression scores were associated with increased CAM use, whilst personality type did not influence rate of use (Table 4).
| Regular CAM use | Mean | SD | SE | 2 tailed P value | |
| Anxiety (HADS) | No | 8.3312 | 3.50750 | 0.09032 | 0.017 |
| Yes | 8.6365 | 3.18002 | 0.08969 | ||
| Depression (HADS) | No | 6.8774 | 2.85105 | 0.07354 | 0.002 |
| Yes | 6.5556 | 2.67318 | 0.07540 | ||
| SIBDQ | No | 56.0152 | 9.71282 | 0.25137 | < 0.001 |
| Yes | 58.1210 | 9.57504 | 0.27126 | ||
| Trait anxiety | No | 21.0042 | 2.53088 | 0.06539 | 0.341 |
| Yes | 21.0957 | 2.48538 | 0.07019 | ||
| Trait curiosity | No | 25.831 | 6.13307 | 0.15836 | 0.916 |
| Yes | 25.8549 | 5.71720 | 0.16158 | ||
| Trait anger | No | 11.3837 | 3.93971 | 0.10169 | 0.385 |
| Yes | 11.5097 | 3.60996 | 0.10202 | ||
| Trait depression | No | 18.9960 | 3.59568 | 0.09293 | 0.744 |
| Yes | 19.0385 | 3.12376 | 0.08818 |
After adjustment for age, gender, disease type and employment level, attitudinal and psychological predictors of regular CAM use using binary logistic regression analysis are shown in Table 5. This model explained a significant proportion of variance in low adherence rates (adjusted pseudo R squared 0.217, goodness of fit Hosmer Lemeshow P = 0.161).
| Odds ratio | 95%CI | P value | |
| Covert dose reduction | 2.588 | 2.135-3.138 | < 0.001 |
| Seeking psychological treatment | 1.888 | 1.563-2.280 | < 0.001 |
| Family and friends are regular CAM users | 1.710 | 1.434-2.044 | < 0.001 |
| Dissatisfied with doctor communication | 1.561 | 1.304-1.869 | < 0.001 |
| Adverse effects conventional medications | 1.208 | 1.006-1.467 | 0.043 |
| Depression (HADS) | 0.910 | 0.878-0.943 | < 0.001 |
| Quality of life (SIBDQ) | 1.022 | 1.011-1.032 | < 0.001 |
After adjustment for demographics a trend was observed toward higher CAM usage amongst non-smokers (OR = 1.299, 95%CI: 0.993-1.698, P = 0.056).
Covert dose reduction, lower depression scores and subjects’ propensity to seek psychological help predicted CAM use, the latter factor analysis generated variable encompassing use of antidepressants, and consultations with counsellors, psychologists or psychiatrists (Table 5). Similarly, the factor analysis generated variable assessing dissatisfaction with doctor communication was an independent predictor of CAM use, and included satisfaction level with doctor relationship, doctor communication style, level of comfort in asking questions of doctor, and comprehension of information provided during consultation.
This study demonstrates the high frequency of CAM use amongst IBD patients in Australia, and suggests that such use occurs independently of health care setting and geography. Newly identified attitudinal and psychological risk factors include dissatisfaction with patient-doctor communication, CAM use by social contacts and lower depression scores. We confirm both the known demographic risk factors for CAM use and known behavioural associations such as covert dose reduction, psychotherapeutic support seeking, and adverse effects of conventional medications.
The frequency of regular CAM use was slightly higher in our study population (45.4%) than reported previously in Australia[4], but within the range reported internationally[1,4,28]. Similarly to the Italian study assessing regional variation in CAM use[14], we found no difference in overall rates of CAM use between cohorts, but in contrast did not find regional variation in the type of CAM chosen either. Some variation in choice of CAM type is seen between populations globally, our predominantly Caucasian cohorts being comparable with New Zealand IBD subjects amongst whom herbs and vitamins were most commonly used[5]. Interestingly nearly two thirds of subjects used more than one type of CAM, however, overlapping physical and homeopathic methods and rendering further analysis by individual CAM type difficult.
Although the patient doctor relationship is known to affect CAM use[29], the more specific aspect of doctor communication quality as a predictor has not been previously reported. Subjects who were dissatisfied with the style of communication from their doctor, did not feel information was presented in a comprehensible way, or felt that the consultation environment did not encourage patient questions, were significantly more likely to use CAM after adjustment for other factors. A Canadian study found that the wish for a more active role in treatment decisions was associated with CAM use[17], and the desire for more information from doctors was predictive of use in an Italian cohort[30].
The significant influence of CAM use behaviours amongst social contacts on CAM uptake decisions in IBD individuals has also not been previously reported. In our study this was adjusted for age, gender, and employment level but not for other demographics which may be common across family members and confound the association. Such influence would not be surprising, however, given the effect of marital status, for example, on other medication taking behaviours such as adherence to conventional therapy in IBD[31]. A study of healthy adolescents found that social contacts exert significant influence over the decision to use CAM[32], and further work to investigate this in IBD populations is warranted, especially given the escalating influence of social media on everyday decision making.
Previously reported predictors including CDR of conventional medications, adverse effects of medications and increased QOL were confirmed in this study. Free text responses strongly suggested that IBD CAM users tend to reduce rather than omit doses of conventional medications on the assumption that CAM use will provide a “medication sparing” effect, the aim being to minimise adverse effects of conventional medications. This newly described phenomenon is the subject of a separate publication[20], which suggests that similar underlying health beliefs and desires drive both CAM uptake and CDR behaviour. Although abundant free text data from this study support this hypothesis, formal path analysis has yet to be undertaken to confirm the direction of causality in the association between CAM use and CDR.
Those subjects seeking psychological input such as counselling, psychologist or psychiatrist review, or antidepressant medication were significantly more likely to use CAM in this study, and this has been previously demonstrated in two European studies[1,13]. Free text responses suggested that CAM was not being prescribed by the psychological care provider, but rather both behaviours were the result of a desire for a holistic health approach with active ways of coping, and this has been previously reported[13]. This may be supported by our new finding that lower depression scores were associated with CAM use, perhaps indicating the presence of successfully treated depression in this population who may be more receptive to psychology.
Gastroenterologist awareness of CAM use was similar in our study to the 46% seen in a French web based study of IBD patients[10], but greater than that found elsewhere[3,8,33]. This communication gap may be contributed to by both consultation participants, a study examining CAM use in IBD patients from the physician perspective finding that only 8% of IBD physicians had initiated CAM conversations themselves, and only around 50% were comfortable discussing CAM with their patients[33].
The confirmation of previously reported demographic and attitudinal CAM predictors suggests that our study population is similar to others, and thus the results generalizable to some extent. The limitations of this study include the small amount of clinical information obtainable from subjects by self-report, including disease activity and response to conventional therapy. Additionally, comparisons between cohorts were hampered by the uneven group sizes and response rates across different treatment settings. Statistical analysis differentiating by CAM type is likely to be important but was not feasible in this study as most subjects (64.5%) reported using more than one therapy type. Also, the definition of CAM is not uniform across studies and in this case was defined as what subjects felt was outside of “conventional” therapy.
CAM use is highly prevalent and appears independent of care setting and geography in IBD, and its importance to patients is often under-recognised by physicians. The quality of patient doctor communication is a key determinant, and failure to actively address CAM use in consultation may promote patient “default” to other advice sources such as family, friends and other social contacts, which ultimately undermines the patient doctor relationship.
The contribution of Ruth Prosser and Sarah Clark (FMC) for their assistance in questionnaire distribution, collection and data entry is greatly appreciated.
Complementary and alternative medicine (CAM) use is common in inflammatory bowel disease (IBD), and some demographic and clinical predictors have been established. This article reports a cross sectional survey of Australian subjects from contrasting care settings with IBD, focussing on the frequency and type of CAM use, and its behavioural and attitudinal predictors.
In the world of ever increasing influence on everyday health decisions from social contacts via social media and the internet, physician understanding of patient context needs to evolve to promote strong and open partnerships with patients in making treatment decisions.
This study demonstrates that patients with IBD make decisions regarding CAM use that are subject to multiple inputs, only one of those inputs being the treating physician. The importance of unqualified health advice from social contacts needs to be acknowledged and addressed in order to optimise adherence to conventional therapy.
IBD physicians need to attend more closely than ever to clear communication with patients regarding the risks and benefits of conventional therapy, and enquire about CAM use to better understand the patient’s context. Patient understanding of disease and therapy should be routinely assessed by physicians in order to correct misperceptions introduced by social contacts, alternative practitioners and the internet that may undermine successful IBD treatment.
This well presented study makes an important contribution to the literature as it highlights the broader context of individuals with IBD, reporting new behavioural predictors of complementary medicine uptake in this population which warrant attention during consultation.
P- Reviewer: Iwasaki Y, Jani K, Shimizu Y, Tasci I S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Lakatos PL, Czegledi Z, David G, Kispal Z, Kiss LS, Palatka K, Kristof T, Nagy F, Salamon A, Demeter P. Association of adherence to therapy and complementary and alternative medicine use with demographic factors and disease phenotype in patients with inflammatory bowel disease. J Crohns Colitis. 2010;4:283-290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Opheim R, Bernklev T, Fagermoen MS, Cvancarova M, Moum B. Use of complementary and alternative medicine in patients with inflammatory bowel disease: results of a cross-sectional study in Norway. Scand J Gastroenterol. 2012;47:1436-1447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Joos S, Rosemann T, Szecsenyi J, Hahn EG, Willich SN, Brinkhaus B. Use of complementary and alternative medicine in Germany - a survey of patients with inflammatory bowel disease. BMC Complement Altern Med. 2006;6:19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 100] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 4. | Leong RW, Lawrance IC, Ching JY, Cheung CM, Fung SS, Ho JN, Philpott J, Wallace AR, Sung JJ. Knowledge, quality of life, and use of complementary and alternative medicine and therapies in inflammatory bowel disease: a comparison of Chinese and Caucasian patients. Dig Dis Sci. 2004;49:1672-1676. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Koning M, Ailabouni R, Gearry RB, Frampton CM, Barclay ML. Use and predictors of oral complementary and alternative medicine by patients with inflammatory bowel disease: a population-based, case-control study. Inflamm Bowel Dis. 2013;19:767-778. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Rawsthorne P, Clara I, Graff LA, Bernstein KI, Carr R, Walker JR, Ediger J, Rogala L, Miller N, Bernstein CN. The Manitoba Inflammatory Bowel Disease Cohort Study: a prospective longitudinal evaluation of the use of complementary and alternative medicine services and products. Gut. 2012;61:521-527. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Ng SC, Lam YT, Tsoi KK, Chan FK, Sung JJ, Wu JC. Systematic review: the efficacy of herbal therapy in inflammatory bowel disease. Aliment Pharmacol Ther. 2013;38:854-863. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 88] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 8. | Park DI, Cha JM, Kim HS, Park HJ, Shin JE, Hong SN, Hong SS, Kim WJ. Predictive factors of complementary and alternative medicine use for patients with inflammatory bowel disease in Korea. Complement Ther Med. 2014;22:87-93. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Opheim R, Hoivik ML, Solberg IC, Moum B. Complementary and alternative medicine in patients with inflammatory bowel disease: the results of a population-based inception cohort study (IBSEN). J Crohns Colitis. 2012;6:345-353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Abitbol V, Lahmek P, Buisson A, Olympie A, Poupardin C, Chaussade S, Lesgourgues B, Nahon S. Impact of complementary and alternative medicine on the quality of life in inflammatory bowel disease: results from a French national survey. Eur J Gastroenterol Hepatol. 2014;26:288-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Agathou CL, Beales IL. Factors associated with the use of probiotics in patients with inflammatory bowel disease. F1000Res. 2013;2:69. [PubMed] [Cited in This Article: ] |
| 12. | Fernández A, Barreiro-de Acosta M, Vallejo N, Iglesias M, Carmona A, González-Portela C, Lorenzo A, Domínguez-Muñoz JE. Complementary and alternative medicine in inflammatory bowel disease patients: frequency and risk factors. Dig Liver Dis. 2012;44:904-908. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Langhorst J, Anthonisen IB, Steder-Neukamm U, Lüdtke R, Spahn G, Michalsen A, Dobos GJ. Amount of systemic steroid medication is a strong predictor for the use of complementary and alternative medicine in patients with inflammatory bowel disease: results from a German national survey. Inflamm Bowel Dis. 2005;11:287-295. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Bertomoro P, Renna S, Cottone M, Riegler G, Bossa F, Giglio L, Pastorelli L, Papi C, Castiglione F, Angelucci E. Regional variations in the use of complementary and alternative medicines (CAM) for inflammatory bowel disease patients in Italy: an IG-IBD study. J Crohns Colitis. 2010;4:291-300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Quattropani C, Ausfeld B, Straumann A, Heer P, Seibold F. Complementary alternative medicine in patients with inflammatory bowel disease: use and attitudes. Scand J Gastroenterol. 2003;38:277-282. [PubMed] [Cited in This Article: ] |
| 16. | Langmead L, Chitnis M, Rampton DS. Use of complementary therapies by patients with IBD may indicate psychosocial distress. Inflamm Bowel Dis. 2002;8:174-179. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 78] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Li FX, Verhoef MJ, Best A, Otley A, Hilsden RJ. Why patients with inflammatory bowel disease use or do not use complementary and alternative medicine: a Canadian national survey. Can J Gastroenterol. 2005;19:567-573. [PubMed] [Cited in This Article: ] |
| 18. | Richardson MA, Mâsse LC, Nanny K, Sanders C. Discrepant views of oncologists and cancer patients on complementary/alternative medicine. Support Care Cancer. 2004;12:797-804. [PubMed] [Cited in This Article: ] |
| 19. | Lui CW, Dower J, Donald M, Coll JR. Patterns and Determinants of Complementary and Alternative Medicine Practitioner Use among Adults with Diabetes in Queensland, Australia. Evid Based Complement Alternat Med. 2012;2012:659419. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3131] [Cited by in F6Publishing: 3208] [Article Influence: 84.4] [Reference Citation Analysis (0)] |
| 21. | Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10:348-354. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1870] [Cited by in F6Publishing: 1910] [Article Influence: 119.4] [Reference Citation Analysis (0)] |
| 22. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28548] [Cited by in F6Publishing: 29363] [Article Influence: 716.2] [Reference Citation Analysis (0)] |
| 23. | Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996;91:1571-1578. [PubMed] [Cited in This Article: ] |
| 24. | Spielberger CD. Cross-cultural assessment of emotional states and personality traits. Europ Psychol. 2006;11:297-303. [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Spielberger C. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press 1970; . [Cited in This Article: ] |
| 26. | Forsberg C, Björvell H. Swedish population norms for the GHRI, HI and STAI-state. Qual Life Res. 1993;2:349-356. [PubMed] [Cited in This Article: ] |
| 27. | Mountifield R, Andrews JM, Mikocka-Walus A, Bampton P. Covert dose reduction is a distinct type of medication non-adherence observed across all care settings in inflammatory bowel disease. J Crohns Colitis. 2014;8:1723-1729. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Weizman AV, Ahn E, Thanabalan R, Leung W, Croitoru K, Silverberg MS, Steinhart AH, Nguyen GC. Characterisation of complementary and alternative medicine use and its impact on medication adherence in inflammatory bowel disease. Aliment Pharmacol Ther. 2012;35:342-349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 29. | Bensoussan M, Jovenin N, Garcia B, Vandromme L, Jolly D, Bouché O, Thiéfin G, Cadiot G. Complementary and alternative medicine use by patients with inflammatory bowel disease: results from a postal survey. Gastroenterol Clin Biol. 2006;30:14-23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | D’Inca R, Garribba AT, Vettorato MG, Martin A, Martines D, Di Leo V, Buda A, Sturniolo GC. Use of alternative and complementary therapies by inflammatory bowel disease patients in an Italian tertiary referral centre. Dig Liver Dis. 2007;39:524-529. [PubMed] [Cited in This Article: ] |
| 31. | Mantzaris GJ, Roussos A, Kalantzis C, Koilakou S, Raptis N, Kalantzis N. How adherent to treatment with azathioprine are patients with Crohn’s disease in long-term remission? Inflamm Bowel Dis. 2007;13:446-450. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Patterson C, Arthur H, Noesgaard C, Caldwell P, Vohra J, Francoeur C, Swinton M. Exploring adolescent complementary/alternative medicine (CAM) use in Canada. J Interprof Care. 2008;22:45-55. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Gallinger Z, Bressler B, Devlin SM, Plamondon S, Nguyen GC. A survey of perceptions and practices of complementary alternative medicine among Canadian gastroenterologists. Can J Gastroenterol Hepatol. 2014;28:45-49. [PubMed] [Cited in This Article: ] |