Abstract
Huntington’s disease (HD) is a neurodegenerative disorder, involving psychiatric, cognitive and motor symptoms, caused by a CAG-repeat expansion encoding an extended polyglutamine tract in the huntingtin protein. Oxidative stress and excitotoxicity have previously been implicated in the pathogenesis of HD. We hypothesized that N-acetylcysteine (NAC) may reduce both excitotoxicity and oxidative stress through its actions on glutamate reuptake and antioxidant capacity. The R6/1 transgenic mouse model of HD was used to investigate the effects of NAC on HD pathology. It was found that chronic NAC administration delayed the onset and progression of motor deficits in R6/1 mice, while having an antidepressant-like effect on both R6/1 and wild-type mice. A deficit in the astrocytic glutamate transporter protein, GLT-1, was found in R6/1 mice. However, this deficit was not ameliorated by NAC, implying that the therapeutic effect of NAC is not due to rescue of the GLT-1 deficit and associated glutamate-induced excitotoxicity. Assessment of mitochondrial function in the striatum and cortex revealed that R6/1 mice show reduced mitochondrial respiratory capacity specific to the striatum. This deficit was rescued by chronic treatment with NAC. There was a selective increase in markers of oxidative damage in mitochondria, which was rescued by NAC. In conclusion, NAC is able to delay the onset of motor deficits in the R6/1 model of Huntington’s disease and it may do so by ameliorating mitochondrial dysfunction. Thus, NAC shows promise as a potential therapeutic agent in HD. Furthermore, our data suggest that NAC may also have broader antidepressant efficacy.
Similar content being viewed by others
Introduction
Huntington’s disease (HD) is an autosomal dominant neurodegenerative disorder resulting from an expanded CAG tandem repeat in the gene encoding huntingtin (HTT).1 The mutant form of HTT includes an expanded polyglutamine tract and elicits progressive psychiatric, cognitive and motor symptoms. A primary neuropathology associated with HD is the selective dysfunction, and eventual death, of medium spiny neurons within the striatum,2, 3, 4 although the cerebral cortex and other areas are also affected. The exact cause of such cellular dysfunction is still unclear, however, it is known that mitochondrial dysfunction, oxidative stress and excitotoxicity have a major role.5, 6, 7, 8 The amino acid, cysteine, has the potential to alleviate each of these features of HD pathology. The compound N-acetylcysteine (NAC) is able to cross the blood–brain barrier and directly donate cysteine to the central nervous system, acting as a potential therapy.9
Oxidative stress has been shown to occur in the brain of patients with HD,5, 6 while an increase in peripheral reactive oxygen species and markers of oxidative stress occur in those in the prodromal phase of the disorder.10 Furthermore, transgenic animal models expressing the amino (N)-terminal fragment of mutant form of Htt show oxidative stress occurring in the striatum before the onset of motor symptoms.11 Cysteine is the rate-limiting amino acid required for the synthesis of glutathione (GSH), the primary endogenous antioxidant in the brain.12 Administration of NAC increases levels of GSH, reducing oxidative stress.13 It has recently been shown that cysteine supplementation is able to alleviate some of the pathology observed in animal models of HD.14
NAC also has the capacity to modulate glutamate-induced toxicity. The elevated synaptic glutamate observed in excitotoxic states leads to dysregulated glutamate receptor activity. Evidence supporting an excitotoxic mechanism in HD includes the development of striatal medium spiny neuron degeneration following the administration of the N-methyl-D-aspartate antagonist, quinolinic acid.15 Furthermore, the R6/2 transgenic mouse model of HD was found to show increased N-methyl-D-aspartate activation before the onset of behavioral phenotypes,16 while the administration of N-methyl-D-aspartate antagonists were found to delay the progression of symptoms in HD patients.17, 18 However, the question remains as to why there is an increased glutamatergic signaling in HD. Astrocytic glutamate uptake may be reduced, leading to an increase in synaptic glutamate. Supporting this, RNA and protein levels of the astrocytic glutamate antiporter, GLT-1 are reduced in postmortem brains of HD patients and transgenic mice.19, 20 Furthermore, treatment with the GLT-1 agonist, ceftriaxone, was found to increase GLT-1 expression and decrease motor abnormalities in the R6/2 mouse model.21 NAC can alleviate excess synaptic glutamate by promoting astrocytic uptake.
Astrocytic glutamate transport can occur via several transporters, two of which are dependent on cysteine: Excitatory amino-acid transporter-1 (also known as GLT-1), which is directly dependent on cysteine and System xc−, which is dependent on cystine derived from oxidized cysteine.22, 23 Supplementation with NAC can both decrease synaptic glutamate and increase intracellular cysteine via these transporters.22, 24, 25 These actions of NAC are therapeutic in models of addiction.26, 27 Given the ability of NAC to increase GSH production and potentially decrease synaptic glutamate via GLT-1, there is the possibility of treating two of the primary neuropathological features of HD: excitotoxicity and oxidative stress. Therefore, the aim of the current study is to test the therapeutic potential of NAC in HD using the R6/1 transgenic mouse model.
Materials and methods
Mice
R6/1 transgenic hemizygote males28 were originally obtained from the Jackson Laboratory (Bar Harbor, ME, USA) and bred with CBB6 (CBA~C57/B6) F1 females to establish the R6/1 colony at the Florey Institute of Neuroscience and Mental Health. After weaning, animals were group housed (four mice per cage with two of each genotype) and maintained on a 12 h light/dark cycle with access to food and water ad libitum. To avoid any possible ‘litter effects’, we ensured that animals from each litter were represented in each experimental condition using appropriate randomization. Experimental animals were kept in open-top cages under standard housing conditions. All the experiments were performed on wild-type (WT) and R6/1 (HD) mice in accordance with the guidelines of the Florey Institute of Neuroscience and Mental Health Animal Ethics Committee and the National Health and Medical Research Council.
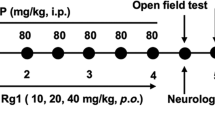
N-Acetylcysteine treatment
N-acetylcysteine (NAC) was obtained from Astral Scientific (#AM0108). NAC was prepared in clinical-grade saline (0.9%) at concentrations suitable for dosing at 500 mg kg−1 per day. Solutions were pH-matched to that of the vehicle (saline). NAC or vehicle were injected intraperitoneally (1 ml per 100 g body weight) daily, beginning at 8 weeks of age and continuing until the mice were culled at 17 weeks of age. NAC and saline treatments were allocated semi-randomly, stratified to ensure that there were no baseline differences in body weight or rotarod performance between treatment groups.
Behavioral analysis
Accelerating rotarod
A rotarod (Ugo Basile model 7650; Sandown Scientific, Hampton, UK) was used as a measure of motor performance. A detailed protocol has been described previously.29 Experimenters were masked to both genotype and treatment. One day before the initial testing phase, mice were acclimatized to the rod; they were allowed to walk at the baseline speed for 2 min before allowing the rod to accelerate to 20 r.p.m. over 150 s. If the mice fell off during this time, they were placed back on the rod until the acclimatization period was complete.
Paw clasping
Mice were held by the tip of the tail against the edge of a table to prevent swinging motion. The mice were observed for a period of 30 s, with the highest clasping score occurring during this time being recorded. Mice were scored on a five-point scale (from 0 to 4) as described previously.30, 31 A score of 0 indicated that no clasping was present, whereas scores from 1 to 4 represented the number of paws clasping. Scorers were masked to both genotype and treatment.
Digigait
Assessment of gait was performed using the Digigait automated treadmill (Mouse Specifics, Boston, MA, USA). On the initial trial, mice were placed inside a plexiglass container on top of a transparent treadmill and allowed to habituate for 1 min. For all time points, the speed of the treadmill was increased incrementally from 0 to 15 cm s−1 over a period of 15 s. Video of the mouse from underneath was then recorded until the mouse ran without stopping for a period of 3 s. The contact of each paw on the treadmill was automatically detected via the Digigait system. Scorers masked to treatment and genotype manually corrected any errors made by the Digigait Software. The major parameters of gait to be analyzed relate to either the ‘duration’ or ‘consistency’ of various stride characteristics. The duration parameters include: total stride, stance, swing, propulsion and brake time. The consistency characteristics include: gait symmetry, paw overlap, paw positioning, stance width and the ataxia coefficient.
Forced swim test
The forced swim test was conducted at 12 weeks of age, as described previously.32 Total immobility time was scored manually by an experienced experimenter masked to both genotype and treatment.
Western blotting
Immediately after cervical dislocation, mice brains were dissected on ice and snap frozen in liquid nitrogen, before being stored at −80 °C. Tissue homogenates were prepared in Tris-lysis buffer containing EDTA, EGTA, glycerol, triton-X100, sodium fluoride, sodium pyrophosphate, Na3VO4, DTT and a protease inhibitor cocktail (Sigma, Castle Hill, NSW, Australia; #p8340). Ribolyser was used at mid-strength for ~10 s with one oscillation per second. Samples were allowed to rest for 10 min on ice before centrifugation at 180 000 g for 25 min at 4 °C. Supernatants were removed and protein concentrations were determined using BCA total protein assay (Thermo, Scoresby, VIC, Australia; #3225). Acrylamide (12%) bis/tris gels were precast and allowed to set at 4 °C overnight. Sample buffer was added to the samples before being heated at 95 °C for 3 min. Samples were then run in tris-glycine buffer using the Bio-Rad (Gladesville, NSW, Australia) MiniPROTEAN Tetra cell system. Gels were transferred to PVDF membrane before being blocked for 1 h in 5% BSA. Blots were washed three times in TBST before incubation in primary antibodies overnight at 4 °C. Primary antibodies were diluted in TBST containing 5% BSA: anti-GLT-1 (1:1000; Millipore, Bayswater, VIC, Australia; #ABN102); anti-xCT (1:500; Abcam, Waterloo, NSW, Australia; #AB37185); and anti-β-actin (1:1000; Cell Signaling Technology, Beverly, MA, USA; #8H10D10). The following day, blots were washed three times in TBST, before being incubated in IR secondary antibodies (1:5000; Li-Cor; Lincoln, NE, USA; #926-3211 and #926-68020) for 1 h at room temperature. Blots were once again washed three times before being imaged in the Li-Cor Odyssey IR detection system. Densitometry was carried out using the integrated intensity value for each band. Analyses of the results were carried out as ratio of protein-of-interest:β-actin.
HPLC
Immediately after cervical dislocation, mice brains were dissected on ice and snap frozen in liquid nitrogen, before being stored at −80 °C. Tissue homogenates were prepared in 0.1% formic acid using a motorized latex pestle for 10 s with one oscillation per second. Samples were then centrifuged at 8000 g for 15 min. The supernatants were then collected and analyzed for levels of reduced and oxidized glutathione (GSH and GSSG, respectively) using the method previously described.33
Protein carbonyl content
Protein carbonyl content was assayed using the Oxyblot kit (Millipore, #S7150). Mitochondrial and nuclear fractions were separated as described previously.34 Nuclear fractions were then prepared in lysis buffer, similarly to whole tissue (see above), while mitochondria were prepared in the mitochondrial isolation buffer. Total protein content was assayed before the preparation of samples. 2,4-Dinitrophenylhydrazine was added to samples to derivatize carbonyl groups from the protein side chains. Derivatized samples were then separated using electrophoresis, as described above. Western blot analysis was carried out, as described above, using the 2,4-dinitrophenylhydrazine antibody provided (1:150). Densitometry was carried out using the integrated intensity value for each band. Analyses of results were carried out as ratio of protein-of-interest:β-actin. Given the presence of multiple bands, the average value of all bands within each lane was used to give an overall measure of protein carbonyl content.
Mitochondrial stress test
All bioenergetic and mitochondrial function analyses were performed using the Seahorse XF24 Extracellular Flux Analyzer (Seahorse Bioscience, Billerica, MA, USA). Immediately after cervical dislocation, the brain was removed and dissected on ice. Samples were then finely chopped in buffer containing mannitol (200 mM), sucrose (50 mM), KH2PO4 (5 mM), EGTA (1 mM), MOPS (5 mM) and BSA (0.1%) to aid in preserving mitochondria. The tissue was then resuspended in the same buffer containing dimethyl sulfoxide (20%), before being slowly frozen on dry ice and stored at −80 °C. Tissue was allowed to defrost on ice before mitochondria were isolated as described previously.34 Mitochondria were then seeded on to 24-well Seahorse V7 plates. Mitochondrial function was determined as previously described35 and basal respiration (state II), adenine diphosphate (ADP)-supplemented respiration with saturated substrate succinate (state III), ADP-deprived respiration (state IV) and respiratory control rate (state III:state IV ratio) were determined from these analyses. Each sample was measured in triplicate, with average values taken from successful wells. Successful wells were those that acted functionally by displaying normal responses to oligomycin (decreased oxygen consumption rate), FCCP (increased oxygen consumption rate) and antimycin A (complete shutdown of oxygen consumption rate). This frozen mitochondria protocol was validated by directly comparing freeze–thaw samples to fresh mitochondrial samples on the same plate. No differences in mitochondrial respiration were found (data not shown).
Statistics
Statistical analyses were performed using IBM SPSS statistics Version 21.0 (IBM, Armonk, NY, USA) and GraphPad Prism 6 (GraphPad Software, La Jolla, CA, USA). Rotarod, clasping, Digigait and body weight data were analyzed using three-way repeated measures analysis of variance. If sphericity was violated, Greenhouse–Geisser corrections were used. If significant interactions were found, alpha-levels for post hoc comparisons were corrected using Bonferroni’s method. All other data were analyzed using two-way analyses of variance. Alpha levels for post hoc comparisons were corrected using Tukey’s honestly significant difference. In all the cases, significance was set at P<0.05.
Results
NAC delays the onset and slows the progression of motor deficits
Paw clasping is a primary motor endophenotype that is observed in the R6 transgenic models of HD.28 A significant interaction of age, treatment and genotype was found on the development of the clasping phenotype (F(9,35)=4.268, P=0.001; Figure 1a). Post hoc analyses revealed that NAC significantly delayed the onset of the clasping phenotype in HD mice. Specifically, saline-treated HD mice differed from control mice from 10 weeks (P=0.017), whereas NAC-treated HD mice did not differ from controls until 14 weeks (P=0.030). Furthermore, NAC-treated HD mice performed significantly better than saline-treated HD mice from 11 weeks (P=0.003) onward, showing reduced clasping scores until the final data point of 17 weeks (P<0.001).
Treatment with NAC delays the onset and progression of motor deficits in HD mice and has antidepressant-like effects in both HD and WT mice. (a) Analysis of the clasping phenotype showed a significant age × treatment × genotype interaction. Post hoc analyses revealed that NAC significantly delayed the onset of the clasping phenotype in HD mice, with saline-HD mice showing clasping behavior from 10 weeks onward, while NAC-HD mice did not show clasping behavior until 14 weeks. NAC-treated HD mice also showed significantly lower levels of clasping behavior relative to saline-treated HD mice from 11 weeks onward. (b) A significant age × treatment interaction was found in Rotarod. Post hoc analyses revealed that the treatment effect began at 12 weeks of age, with NAC-HD mice performing better than saline-HD mice from 11 weeks of age. There was also a significant age × genotype interaction, with post hoc analyses revealing that genotype deficits were present from 8 weeks of age, progressively worsening over the lifespan of the mice. (c) Representation of the different phases of stride that can be measured using the Digigait, including total stride, stance, swing, brake and propel duration. (d) A significant treatment × genotype interaction was found in the propel/brake ratio. Post hoc tests show that saline-HD mice have a higher ratio than both NAC-HD and saline-WT mice. (e) A significant treatment effect was seen in the time spent immobile during the FST, with NAC-treated mice spending less time immobile than saline-treated mice. Error bars represent mean±s.e.m.; n=10–14; treatment effects: *P<0.05, **P<0.01, ***P<0.001. FST, forced swim test; HD, Huntington’s disease; NAC, N-acetylcysteine; WT, wild type.
The Rotarod was also used to assess motor coordination, and revealed a significant interaction of age and genotype (F(9,35)=7.993, P<0.001). Post hoc analyses revealed that HD mice displayed rotarod deficits from baseline (8 weeks; P=0.001) and progressively worsened until 17 weeks (P<0.001). However, a significant interaction of treatment and age was also observed (F(9,35)=2.746, P=0.015; Figure 1b). Post hoc analyses show that NAC-treated HD mice performed better than saline-treated HD mice from 11 weeks (P=0.038) of age onward.
In a separate analysis of the lower dose of 250 mg kg−1 per day (data not shown), a significant age × genotype interaction was also found (F(7,33)=6.191, P<0.001), with the HD mice showing deficits by 10 weeks (P=0.012) and progressively worsening until 17 weeks (P<0.001). A significant main effect of treatment was also seen at the lower dose (F(1,39)=4.974, P=0.039).
NAC rescues gait abnormalities
The Digigait behavioral apparatus was used to assess if NAC rescues gait abnormalities present in R6/1 mice. Mice were assessed at 8, 10, 12 and 14 weeks of age. Later time points were not measured as HD mice were unable to perform the task due to the progressive degeneration. The session conducted at the 8-week time point was taken as a training session, so measurements were not included in the end analysis. At this time point all groups show movement patterns that are consistent with a motor learning phase (Supplementary Figures 1a and b). Overall, the duration of each phase of movement of the hind paws were found to be the more sensitive indicators of gait abnormalities in HD mice, therefore, the following data are specific to hind paws only.
The time spent in each phase of the stride can be broken down into the following: total stride, stance, swing, propulsion and brake time (as shown in Figure 1c). Significant interactions between age and genotype are present in stride, stance and swing duration (F(2,34)=7.841, P=0.002; F(2,34)=5.918, P=0.006; F(2,34)=4.941, P=0.010; Supplementary Figures 1d and f). Post hoc tests reveal that for each parameter, measurements for WT mice increased from 12 to 14 weeks (P=0.027; P=0.016; and P=0.027, respectively), while HD mice decreased in stride duration from 12 to 14 weeks (P=0.022). Within stance, no changes were found in the time spent propelling (data not shown), whereas a significant interaction of treatment and genotype was found in the time spent braking (F(1,35)=9.728, P=0.004; Supplementary Figure 1c). Post hoc comparisons revealed that saline-treated HD mice had lower braking time than controls (P=0.014), whereas NAC-treated HD mice showed no differences relative to controls. A significant interaction of age and genotype was also found (F(2,34)=4.399; P=0.010), with HD mice showing decreased brake duration at 14 weeks (P=0.012), but no difference at 10–12 weeks. A significant interaction of treatment and genotype was found in the propel/brake ratio (F(1,35)=9.841, P=0.003; Figure 1d). Post hoc tests revealed that saline-treated HD mice show an increased ratio compared with both NAC-treated HD mice (P=0.046) and controls (P=0.002), whereas NAC-treated HD mice showed no difference to controls. No changes were found in gait symmetry, paw overlap, paw positioning, stance width and the ataxia coefficient (data not shown).
NAC reduces immobility during forced swim
The time spent immobile during a period of forced swim was used as a measure of learned helplessness. No differences were found between genotypes. However, a significant effect of treatment was found (F(1,44)=5.739, P=0.021), with NAC-treated mice having lower immobility time than saline-treated mice (Figure 1e). This effect was replicated at a lower dose of 250 mg kg−1 (F(1,23)=5.992, P=0.022), with NAC-treated mice having lower immobility time than saline-treated mice (data not shown).
Change in brain weight, but not body weight, is rescued by NAC
A significant interaction of genotype and treatment was found in brain weight (F(1,43)=9.428; P=0.004). NAC-treated HD mice were found to have heavier brains than saline-treated HD mice (P<0.001), whereas both WT mice had heavier brains than both saline and NAC-treated HD mice (P<0.001 for each comparison; Figure 2a). A significant interaction of age and genotype was found (F(9,35)=16.763; P<0.001), with body weights of HD mice declining from 13 weeks (Figure 2b). However, no differences were noted due to treatment.
NAC affects brain weight but not body weight of R6/1 mice. (a) A significant interaction between genotype and treatment was found in the brain weight of 17-week-old mice. Post hoc analyses revealed that saline-treated HD mice had significantly lower brain weights than WT mice, and NAC partially restored this. (b) A significant age × genotype interaction was found in body weight. Post hoc tests revealed that the genotype difference began at 12 weeks of age and progressively increased until 17 weeks. Error bars represent mean±s.e.m.; n=10–14; treatment effects: ***P<0.001. HD, Huntington’s disease; NAC, N-acetylcysteine; WT, wild type.
NAC does not affect glutamate transporters
Western blot analysis was carried out on striatal and cortical samples from 17-week-old mice. GLT-1 levels were found to be reduced in the striatum and cortex of HD mice (F(1,24)=6.032, P=0.029; and F(1,24)=15.03, P<0.001, respectively), however, this deficit was not rescued by NAC (Figures 3a and b). The light chain of System xc−, denoted xCT, confers substrate specificity,36 hence, protein levels of xCT were measured as an index of System xc− expression (Figures 3c and d). No changes in xCT were found across genotype or treatment groups in either the striatum or cortex.
Western blot analysis of astrocytic glutamate transporter proteins in the striatum and cortex. (a–b) GLT-1 was significantly reduced in the striatum and cortex of HD mice, but was unaffected by NAC treatment. (c–d) Protein levels of xCT were unchanged across genotype and treatment. Error bars represent mean±s.e.m.; n=7–8; genotype effects: #P<0.05. HD, Huntington’s disease; NAC, N-acetylcysteine; WT, wild type.
NAC has mitochondria-specific antioxidant effects
GSH is one of the primary endogenous antioxidants. When GSH is oxidized, it forms glutathione disulfide (GSSG). By looking at the ratio of GSH:GSSG, the antioxidant capacity of the cell can be inferred.9 To assess the antioxidant capacity of the striatum, GSH and GSSG were measured via HPLC. No changes in either GSH, GSSG or the GSH:GSSG ratio were found (Supplementary Figure 2).
As the effects of oxidative stress may differ across cellular compartments, the striatal tissue of 17-week-old mice was separated into mitochondrial and nuclear fractions. Protein carbonylation is a stable indicator of oxidative damage to proteins.37 Within the nuclear fraction of the striatum, no difference in protein carbonylation was found within either genotype or treatment groups (Figure 4b). In contrast, the analysis of protein carbonylation in striatal mitochondria revealed a significant interaction between genotype and treatment (F(1,26)=8.864, P=0.006; Figure 5a). Post hoc comparisons show that there is a two-fold increase in protein oxidation in HD mice (P<0.01), which NAC is able to completely rescue (P<0.05). No differences in protein carbonylation were found between the treatment or genotype groups, in either the nuclear or mitochondrial fraction of cortical tissue (Figures 4c and d).
Oxidative stress as assayed by protein carbonyl content in fractions of striatal and cortical tissue. (a) There was a significant interaction between genotype and treatment in protein carbonyl content within the striatal mitochondria. Post hoc comparisons revealed that saline-HD mitochondria had higher protein carbonyl content than saline-WT and this was rescued in NAC-HD mice. (b–d) There were no differences in protein carbonyl content in the mitochondrial fraction of the cortex, or in the nuclear fractions from the striatum and cortex across either genotype or treatment groups. Error bars represent mean±s.e.m.; n=7–8; genotype and treatment effects: ##P<0.01 and *P<0.05, respectively. HD, Huntington’s disease; NAC, N-acetylcysteine; WT, wild type.
Functional analysis of mitochondria isolated from the striatum and cortex. (a) Overview of the results from the mitochondrial stress test performed on the striatal mitochondria, where it was found that: (b–d) State II, state III and state IV respiration, all displayed significant interactions. Post hoc tests all showed that saline-HD mitochondria had lower respiration than saline-WT. NAC-HD mitochondria did not differ from saline-WT mitochondria in any respiratory state. (e) A significant genotype effect was found in the state III:state II ratio, with HD mitochondria higher than WT. (f) No differences in RCR were found in the striatal mitochondria. (g) Overview of the results from the mitochondrial stress test performed on the cortical mitochondria, where it was found that: (h–l) state II, state III and state IV respiration, the state III:state II ratio and RCR, did not differ between groups. Error bars represent mean±s.e.m.; n=7–8; genotype effects: *P<0.05; ##P<0.01. HD, Huntington’s disease; NAC, N-acetylcysteine; RCR, respiratory control rate; WT, wild type.
NAC rescues functional deficits in HD mitochondria
Mitochondria were isolated from the striatum and cortex and a mitochondrial stress test was performed to assess their function. Mitochondria isolated from the striatum show differences in state II, state III and state IV respiration, and the state III:state II ratio (Figure 5a). Specifically, a significant interaction was found in state II respiration (F(1,18)=8.078, P=0.011), with post hoc tests revealing that saline-treated HD mitochondria had lower state II respiration than saline-treated WT mitochondria (P<0.05). A significant interaction was also found in state III and state IV respiration (F(1,18)=9.409, P=0.007; and F=6.738, P=0.018, respectively), with post hoc tests revealing that saline-treated HD mitochondria had lower state III and state IV respiration than saline-treated WT mitochondria (P<0.05). Furthermore, a genotype effect was found on the state III:state II ratio (F(1,18)=10.85, P=0.004), with HD mitochondria showing a higher ratio than WT. No changes were found in the respiratory control rate. Mitochondria isolated from the cortex show no differences across treatment or genotype groups on any measures of respiration (Figures 2g and l).
Discussion
Motor dysfunction is a primary clinical symptom of HD. In this study, we show that NAC is able to delay the onset, and slow the progression, of motor symptoms in a transgenic mouse model of HD. Depressive symptoms are also common in HD38 and we show that NAC displays antidepressant-like effects in both HD and WT mice. NAC was found to rescue oxidative stress within striatal mitochondria of HD mice. These changes were associated with rescued functional deficits in the mitochondria. This supports the hypothesis that NAC rescues motor dysfunction by ameliorating mitochondrial dysfunction and inhibiting oxidative stress.
We have employed a comprehensive analysis of R6/1 motor deficits to assess the domains that are rescued by NAC. Uncontrolled and reflexive paw-clasping is a primary motor endophenotype shown by the R6 transgenic mice.28 NAC was able to substantially delay the onset of paw-clasping in HD mice, and significantly reduce the severity of this abnormal phenotype. Similar effects were also seen in rotarod performance.
The rotarod is the most widely used tool to test motor performance in HD mice. The rotarod primarily tests locomotor coordination, with R6/1 mice displaying a progressive deficit in their performance.39 R6/1 mice were treated with NAC after the onset of this deficit; however, the drug was still able to significantly inhibit the progressive loss of locomotor coordination. It is striking that NAC was able to take effect even in animals that had already undergone some loss of striatal function. In contrast, NAC has been shown previously to have detrimental effects in fly and zebrafish models of HD40 when administered before the development of HD phenotypes. This was shown to be due to an inhibition of autophagy clearance of mutant HTT aggregates. It may be that the therapeutic benefit of NAC outweighs possible detriments after the pathological hallmarks have developed,41 although it is difficult to directly compare dosing regimes across such divergent model species. Similar dichotomous effects have also been seen in HD models using other paradigms such as stress, where corticosterone treatment was found to hasten the onset of cognitive symptoms in presymptomatic R6/1 mice42 whereas dexamethasone (a synthetic glucocorticoid) administration was able to increase heat-shock response, reduce mutant HTT aggregate load and slow the progression of motor dysfunction in the more severe R6/2 model of HD.43 Furthermore, evidence for the therapeutic effects of NAC in HD mice expressing a human transgene is likely to be more clinically relevant than the data from transgenic fish and flies. Thus, NAC has advantages for potential clinical application of this therapy, where diagnosis and treatment are typically commenced after the development of analogous motor symptoms.
The therapeutic effects of NAC were also mirrored in the gait analysis of R6/1 mice. The Digigait analysis has only been published once previously in a HD mouse model, in which Pallier et al.44 conducted a cross-sectional analysis of gait in late-stage R6/2 mice (17 weeks). We are the first to report a progressive analysis of gait in a HD animal model, beginning at the time of motor symptom onset. Overall, R6/1 mice show an emerging deficit in two components of stance: time spent braking and the brake-to-propel ratio. Specifically, HD mice display a decrease in the time spent braking, with a subsequent increase in the propel-to-brake ratio. These findings are consistent with Pallier et al., who found deficits within ‘stance’ components only. Importantly, we found that NAC was able to rescue these deficits. Thus, with the treatment of NAC, we were able to rescue deficits in R6/1 mice from three separate domains of motor function: reflexive paw-clasping, locomotor coordination and gait. NAC also had antidepressant-like effects.
Depression is the highest occurring psychiatric comorbidity in HD,38 with recent studies suggesting that it is an inherent symptom of the disorder.45 Immobility time during the forced swim test is the gold standard for screening the efficacy of antidepressants in rodents.46 We found that NAC was able to reduce the time spent immobile in both R6/1 mice and their wild-type littermates. This has implications for both HD and wider research on major depression, suggesting that NAC may be an effective antidepressant. This supports data from previous clinical studies on bipolar patients, which have shown NAC to have positive effects on the depressive symptoms of the disorder.47 Taken together, NAC was able to display antidepressant-like effects, while also rescuing an array of motor deficits in the R6/1 mice. Our findings are echoed by a recent publication displaying the ability of cysteine supplementation to reverse clasping and Rotarod deficits within the R6/2 model of HD—although gait and affective-like behaviors were not assessed.14 In this study, cysteine supplementation was given using a cysteine-rich diet in combination with NAC. Our study is the first to display the therapeutic effect of NAC alone in a transgenic animal model.
NAC may be acting in the brain through modulation of glutamatergic excitotoxicity or levels of oxidative stress. Glutamate-dependent toxicity is an established mechanism of cellular dysfunction within both HD patients and animal models.7, 48, 49, 50 Glutamate can be transported out of the synapse by a variety of excitatory amino-acid transporters, including the astrocytic transporter, GLT-1.24 GLT-1-dependent glutamate uptake is impeded by the presence of a high extracellular glutamate-to-cysteine ratio.24, 25 Therefore, the increase in synaptic glutamate may explain why GLT-1 is decreased in HD.19, 20, 51 Our findings replicate previous studies19, 52 showing a deficit in striatal and cortical GLT-1, however, NAC did not rescue this change.
NAC is also capable of acting on a second astrocytic glutamate transporter, System xc−.23 System xc− is responsible for the transport of glutamate from astrocytes in a 1:1 exchange for extracellular cysteine.22, 53 Cystine is produced by creating a disulfide bond through the oxidation of two cysteine groups, and is thus dependent on extracellular levels of cysteine.24 Previous studies have shown that NAC is able to upregulate glutamate–cysteine exchange, and this has a therapeutic effect in treating drug withdrawal in animals and humans.26, 54 The light chain of System xc−, xCT, confers substrate specificity, thus protein levels of xCT were analyzed to evaluate functional changes in System xc−. No changes were found in levels of xCT. Considering GLT-1 and System xc− are the only glutamate transporters dependent on the presence of extracellular cysteine, we can conclude that the mechanism of action of NAC in R6/1 mice is not directly related to the reduction of glutamate-dependent toxicity. We, therefore, hypothesized that NAC is functioning by reducing oxidative stress.
GSH is the primary endogenous antioxidant.55 When GSH is oxidized, it forms GSSG.55 By looking at the ratio of GSH:GSSG, the antioxidant capacity of the cell can be inferred.9 Previous studies in HD have shown that GSH is reduced in the serum of HD patients.10 However, other studies have shown that GSH and GSSG are unchanged in R6/1 mouse striatum at the onset of motor symptoms.33 NAC could potentially stabilize the GSH:GSSG balance by donating cysteine for the synthesis of new GSH.56 We observed no changes in either GSH, GSSG or the GSH:GSSG ratio in unfractionated tissue homogenates. However, the levels of these key elements of the antioxidant system are differentially regulated across cellular organelles.
GSH is produced in the cytosol and transferred to other intracellular components, such as nuclei and mitochondria.57, 58 Thus, although the total GSH/GSSG pools may be unchanged at the level of the whole tissue, it may be that oxidative stress is occurring in specific organelles of the cell. To investigate the possibility of compartmentalized oxidative stress, the striatal and cortical tissue of 17-week-old mice were fractionated into mitochondrial and nuclear components. Given the volatile nature of the GSH-GSSG redox cycle, as well as the reactive nature of GSH to oxidation, it may be that subtle differences in GSH:GSSG are quickly lost in the postmortem brain.59 Therefore, protein carbonylation was assessed as a more stable indicator of oxidative damage to proteins.37 It was found that this key marker of damage resulting from oxidative stress was increased in mitochondrial, but not nuclear, fractions of striatal tissue only. Importantly, NAC was able to rescue this region- and organelle-specific oxidative stress.
It has been shown previously that mitochondria are more prone to oxidative damage than nuclei within immortalized striatal cells from HdhQ111/Q111 mice.60 This is to be expected given that mitochondria are the primary source of reactive oxygen species within the cell.61 Mitochondria are more likely to leak reactive oxygen species when they are not functioning efficiently.61 Multiple studies have shown mitochondrial processes to be dysfunctional in HD, including reductions in the activity of electron transport chain complexes II, III and IV,6, 48, 62, 63 as well as reduced activity of aconitase,50 pyruvate dehydrogenase64 and creatine kinase.65 Each of these studies are beneficial in showing reductions in activity of specific enzymes, however, the electron transport chain contains dynamic protein complexes, and isolation of specific enzymes cannot elucidate the overall mitochondrial function. Thus, we sought to look at the respiratory function of intact mitochondria isolated from the striatum of R6/1 mice. We hypothesized that the oxidative stress specific to the R6/1 mitochondria would be associated with an overall reduction in mitochondrial oxidative metabolism, which would be rescued by NAC treatment.
To assess mitochondrial function, oxygen consumption rates were assessed after the administration of various mitochondrial substrates and inhibitors. This analysis showed that NAC enhanced baseline respiration (state II), maximal ADP-stimulated respiration (state III) and respiration after consumption of ADP (state IV), in HD mice, suggesting that NAC could enhance mitochondrial capacity in this model. This provides functional evidence to support the finding that ATP pools are depleted in HD models.66 This also has potential implications for the generation of mitochondrial reactive oxygen species, a putative pathogenic factor in HD. Lower capacity for ADP-stimulated respiration, in the face of constant energy demand and substrate supply, increases the mitochondrial membrane potential. Electron leak from the respiratory chain in the form of O2− is a compensatory response to limit further increases in membrane potential, resulting in an oxidative stress response.67 Indeed, the enhanced respiratory capacity of HD mice treated with NAC was associated with lower protein carbonylation in mitochondrial fractions from HD mice and could have protected from further mitochondrial oxidative damage and dysfunction.
Taken together, NAC was found to delay the onset and progression of motor dysfunction in the R6/1 transgenic mouse model of HD, while displaying antidepressant-like effects on both R6/1 and WT mice. NAC was also shown to rescue mitochondrial dysfunction and reduce oxidative stress within the R6/1 striatum, identifying a likely mechanism of action. Considering that NAC is established as safe for clinical use,68 our data suggest that it should be considered as a candidate for trial as either a primary or adjunctive treatment for symptomatic HD patients. The question of whether NAC would be effective in presymptomatic stages of the disease is also a high priority for investigation, and it is suggested that trialing NAC on a slower progressing model, such as knock-in or BACHD mice, would provide more insight, as there are no disease-modifying therapies currently available for this devastating disorder.
References
MacDonald ME, Ambrose CM, Duyao MP, Myers RH, Lin C, Srinidhi L et al. A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington's disease chromosomes. Cell 1993; 72: 971–983.
Vonsattel JP, Myers RH, Stevens TJ, Ferrante RJ, Bird ED, Richardson EP Jr . Neuropathological classification of Huntington's disease. J Neuropathol Exp Neurol 1985; 44: 559–577.
Ferrante RJ, Kowall NW, Beal MF, Richardson EP Jr, Bird ED, Martin JB . Selective sparing of a class of striatal neurons in Huntington's disease. Science 1985; 230: 561–563.
Graveland GA, Williams RS, DiFiglia M . Evidence for degenerative and regenerative changes in neostriatal spiny neurons in Huntington's disease. Science 1985; 227: 770–773.
Browne SE, Ferrante RJ, Beal MF . Oxidative stress in Huntington's disease. Brain Pathol 1999; 9: 147–163.
Browne SE, Bowling AC, MacGarvey U, Baik MJ, Berger SC, Muqit MM et al. Oxidative damage and metabolic dysfunction in Huntington's disease: selective vulnerability of the basal ganglia. Ann Neurol 1997; 41: 646–653.
Tabrizi SJ, Cleeter MW, Xuereb J, Taanman JW, Cooper JM, Schapira AH . Biochemical abnormalities and excitotoxicity in Huntington's disease brain. Ann Neurol 1999; 45: 25–32.
Estrada Sanchez AM, Mejia-Toiber J, Massieu L . Excitotoxic neuronal death and the pathogenesis of Huntington's disease. Arch Med Res 2008; 39: 265–276.
Dean O, Giorlando F, Berk M . N-acetylcysteine in psychiatry: current therapeutic evidence and potential mechanisms of action. J Psychiatry Neurosci 2011; 36: 78–86.
Klepac N, Relja M, Klepac R, Hecimovic S, Babic T, Trkulja V . Oxidative stress parameters in plasma of Huntington's disease patients, asymptomatic Huntington's disease gene carriers and healthy subjects: a cross-sectional study. J Neurol 2007; 254: 1676–1683.
Bogdanov MB, Andreassen OA, Dedeoglu A, Ferrante RJ, Beal MF . Increased oxidative damage to DNA in a transgenic mouse model of Huntington's disease. J Neurochem 2001; 79: 1246–1249.
Aruoma OI, Halliwell B, Hoey BM, Butler J . The antioxidant action of N-acetylcysteine: its reaction with hydrogen peroxide, hydroxyl radical, superoxide, and hypochlorous acid. Free Radic Biol Med 1989; 6: 593–597.
Atkuri KR, Mantovani JJ, Herzenberg LA, Herzenberg LA . N-Acetylcysteine—a safe antidote for cysteine/glutathione deficiency. Curr Opin Pharmacol 2007; 7: 355–359.
Paul BD, Sbodio JI, Xu R, Vandiver MS, Cha JY, Snowman AM et al. Cystathionine [ggr]-lyase deficiency mediates neurodegeneration in Huntington's disease. Nature 2014; 509: 96–100.
Portera-Cailliau C, Hedreen JC, Price DL, Koliatsos VE . Evidence for apoptotic cell death in Huntington disease and excitotoxic animal models. J Neurosci 1995; 15: 3775–3787.
Cepeda C, Hurst RS, Calvert CR, Hernandez-Echeagaray E, Nguyen OK, Jocoy E et al. Transient and progressive electrophysiological alterations in the corticostriatal pathway in a mouse model of Huntington's disease. J Neurosci 2003; 23: 961–969.
Lucetti C, Gambaccini G, Bernardini S, Dell'Agnello G, Petrozzi L, Rossi G et al. Amantadine in Huntington's disease: open-label video-blinded study. Neurol Sci 2002; 23: S83–S84.
Beister A, Kraus P, Kuhn W, Dose M, Weindl A, Gerlach M . The N-methyl-D-aspartate antagonist memantine retards progression of Huntington’s disease. In: Müller T, Riederer P (eds). Focus on Extrapyramidal Dysfunction, vol. 68. Springer: Vienna, 2004, pp 117-22.
Lievens JC, Woodman B, Mahal A, Spasic-Boscovic O, Samuel D, Kerkerian-Le Goff L et al. Impaired glutamate uptake in the R6 Huntington's disease transgenic mice. Neurobiol Dis 2001; 8: 807–821.
Behrens PF, Franz P, Woodman B, Lindenberg KS, Landwehrmeyer GB . Impaired glutamate transport and glutamate-glutamine cycling: downstream effects of the Huntington mutation. Brain 2002; 125: 1908–1922.
Sari Y, Prieto AL, Barton SJ, Miller BR, Rebec GV . Ceftriaxone-induced up-regulation of cortical and striatal GLT1 in the R6/2 model of Huntington's disease. J Biomed Sci 2010; 17: 62.
McBean GJ . Cerebral cystine uptake: a tale of two transporters. Trends Pharmacol Sci 2002; 23: 299–302.
Sanacora G, Banasr M . From pathophysiology to novel antidepressant drugs: glial contributions to the pathology and treatment of mood disorders. Biol Psychiatry 2013; 73: 1172–1179.
McBean GJ, Flynn J . Molecular mechanisms of cystine transport. Biochem Soc Trans 2001; 29: 717–722.
Bender AS, Reichelt W, Norenberg MD . Characterization of cystine uptake in cultured astrocytes. Neurochem Int 2000; 37: 269–276.
Moussawi K, Pacchioni A, Moran M, Olive MF, Gass JT, Lavin A et al. N-Acetylcysteine reverses cocaine-induced metaplasticity. Nat Neurosci 2009; 12: 182–189.
Kupchik YM, Moussawi K, Tang X-C, Wang X, Kalivas BC, Kolokithas R et al. The effect of N-acetylcysteine in the nucleus accumbens on neurotransmission and relapse to cocaine. Biol Psychiatry 2012; 71: 978–986.
Mangiarini L, Sathasivam K, Seller M, Cozens B, Harper A, Hetherington C et al. Exon 1 of the HD gene with an expanded CAG repeat is sufficient to cause a progressive neurological phenotype in transgenic mice. Cell 1996; 87: 493–506.
van Dellen A, Cordery PM, Spires TL, Blakemore C, Hannan AJ . Wheel running from a juvenile age delays onset of specific motor deficits but does not alter protein aggregate density in a mouse model of Huntington's disease. BMC Neurosci 2008; 9: 34.
Miller BR, Dorner JL, Shou M, Sari Y, Barton SJ, Sengelaub DR et al. Up-regulation of GLT1 expression increases glutamate uptake and attenuates the Huntington's disease phenotype in the R6/2 mouse. Neuroscience 2008; 153: 329–337.
Petr GT, Schultheis LA, Hussey KC, Sun Y, Dubinsky JM, Aoki C et al. Decreased expression of GLT-1 in the R6/2 model of Huntington's disease does not worsen disease progression. Eur J Neurosci 2013; 38: 2477–2490.
Renoir T, Zajac MS, Du X, Pang T, Leang L, Chevarin C et al. Sexually dimorphic serotonergic dysfunction in a mouse model of Huntington’s disease and depression. PLoS One 2011; 6: e22133.
Smith ZM, Terry JM, Barnett NW, Gray LJ, Wright DJ, Francis PS . Enhancing permanganate chemiluminescence detection for the determination of glutathione and glutathione disulfide in biological matrices. Analyst 2014; 139: 2416–2422.
Rogers GW, Brand MD, Petrosyan S, Ashok D, Elorza AA, Ferrick DA et al. High throughput microplate respiratory measurements using minimal quantities of isolated mitochondria. PLoS One 2011; 6: e21746.
McGee SL, Sadli N, Morrison S, Swinton C, Suphioglu C . DHA protects against zinc mediated alterations in neuronal cellular bioenergetics. Cell Physiol Biochem 2011; 28: 157–162.
Bannai S, Christensen HN, Vadgama JV, Ellory JC, Englesberg E, Guidotti GG et al. Amino acid transport systems. Nature 1984; 311: 308.
Dalle-Donne I, Rossi R, Giustarini D, Milzani A, Colombo R . Protein carbonyl groups as biomarkers of oxidative stress. Clin Chim Acta 2003; 329: 23–38.
Slaughter JR, Martens MP, Slaughter KA . Depression and Huntington's disease: prevalence, clinical manifestations, etiology, and treatment. CNS Spectr 2001; 6: 306–326.
Carter RJ, Lione LA, Humby T, Mangiarini L, Mahal A, Bates GP et al. Characterization of progressive motor deficits in mice transgenic for the human Huntington's disease mutation. J Neurosci 1999; 19: 3248–3257.
Underwood BR, Imarisio S, Fleming A, Rose C, Krishna G, Heard P et al. Antioxidants can inhibit basal autophagy and enhance neurodegeneration in models of polyglutamine disease. Hum Mol Genet 2010; 19: 3413–3429.
Ma YT, Galluzzi L, Zitvogel L, Kroemer G . Autophagy and cellular immune responses. Immunity 2013; 39: 211–227.
Mo C, Pang TY, Ransome MI, Hill RA, Renoir T, Hannan AJ . High stress hormone levels accelerate the onset of memory deficits in male Huntington's disease mice. Neurobiol Dis 2014; 69: 248–262.
Maheshwari M, Bhutani S, Das A, Mukherjee R, Sharma A, Kino Y et al. Dexamethasone induces heat shock response and slows down disease progression in mouse and fly models of Huntingtons disease. Hum Mol Genet 2014; 23: 2737–2751.
Pallier PN, Drew CJG, Morton AJ . The detection and measurement of locomotor deficits in a transgenic mouse model of Huntington's disease are task- and protocol-dependent: influence of non-motor factors on locomotor function. Brain Res Bull 2009; 78: 347–355.
Du X, Pang TYC, Hannan AJ . A tale of two maladies? Pathogenesis of depression with and without the Huntington's disease gene mutation. Front Neurol 2013; 4: 81.
Overstreet DH . Modeling depression in animal models. Methods Mol Biol 2012; 829: 125–144.
Berk M, Copolov DL, Dean O, Lu K, Jeavons S, Schapkaitz I et al. N-acetyl cysteine for depressive symptoms in bipolar disorder—a double-blind randomized placebo-controlled trial. Biol Psychiatry 2008; 64: 468–475.
Gu M, Gash MT, Mann VM, Javoy-Agid F, Cooper JM, Schapira AH . Mitochondrial defect in Huntington's disease caudate nucleus. Ann Neurol 1996; 39: 385–389.
Grunewald T, Beal MF . Bioenergetics in Huntington's disease. Ann N Y Acad Sci 1999; 893: 203–213.
Tabrizi SJ, Workman J, Hart PE, Mangiarini L, Mahal A, Bates G et al. Mitochondrial dysfunction and free radical damage in the Huntington R6/2 transgenic mouse. Ann Neurol 2000; 47: 80–86.
Faideau M, Kim J, Cormier K, Gilmore R, Welch M, Auregan G et al. In vivo expression of polyglutamine-expanded huntingtin by mouse striatal astrocytes impairs glutamate transport: a correlation with Huntington's disease subjects. Hum Mol Genet 2010; 19: 3053–3067.
Estrada-Sanchez AM, Montiel T, Segovia J, Massieu L . Glutamate toxicity in the striatum of the R6/2 Huntington's disease transgenic mice is age-dependent and correlates with decreased levels of glutamate transporters. Neurobiol Dis 2009; 34: 78–86.
Lewerenz J, Hewett SJ, Huang Y, Lambros M, Gout PW, Kalivas PW et al. The cystine/glutamate antiporter system x(c)(-) in health and disease: from molecular mechanisms to novel therapeutic opportunities. Antioxid Redox Signal 2013; 18: 522–555.
Knackstedt LA, LaRowe S, Mardikian P, Malcolm R, Upadhyaya H, Hedden S et al. The role of cystine-glutamate exchange in nicotine dependence in rats and humans. Biol Psychiatry 2009; 65: 841–845.
Dringen R, Hirrlinger J . Glutathione pathways in the brain. Biol Chem 2003; 384: 505–516.
Berk M, Malhi GS, Gray LJ, Dean OM . The promise of N-acetylcysteine in neuropsychiatry. Trends Pharmacol Sci 2013; 34: 167–177.
Garcia O, Almeida A, Massieu L, Bolanos JP . Increased mitochondrial respiration maintains the mitochondrial membrane potential and promotes survival of cerebellar neurons in an endogenous model of glutamate receptor activation. J Neurochem 2005; 92: 183–190.
Wadey AL, Muyderman H, Kwek PT, Sims NR . Mitochondrial glutathione uptake: characterization in isolated brain mitochondria and astrocytes in culture. J Neurochem 2009; 109: 101–108.
Perry TL, Hansen S, Gandham SS . Postmortem changes of amino compounds in human and rat brain. J Neurochem 1981; 36: 406–410.
Siddiqui A, Rivera-Sanchez S, Castro MDR, Acevedo-Torres K, Rane A, Torres-Ramos CA et al. Mitochondrial DNA damage is associated with reduced mitochondrial bioenergetics in Huntington's disease. Free Radic Biol Med 2012; 53: 1478–1488.
Turrens JF . Mitochondrial formation of reactive oxygen species. J Physiol 2003; 552: 335–344.
Brennan WA Jr ., Bird ED, Aprille JR . Regional mitochondrial respiratory activity in Huntington's disease brain. J Neurochem 1985; 44: 1948–1950.
Benchoua A, Trioulier Y, Zala D, Gaillard M-C, Lefort N, Dufour N et al. Involvement of mitochondrial complex II defects in neuronal death produced by N-terminus fragment of mutated huntingtin. Mol Biol Cell 2006; 17: 1652–1663.
Butterworth J, Yates CM, Reynolds GP . Distribution of phosphate- activated glutaminase, succinic dehydrogenase, pyruvate dehydrogenase andgamma-glutamyl transpeptidase in post-mortem brain from Huntington's disease and agonal cases. J Neurol Sci 1985; 67: 161–171.
Zhang SF, Hennessey T, Yang L, Starkova NN, Beal MF, Starkov AA . Impaired brain creatine kinase activity in Huntington's disease. Neurodegener Dis 2011; 8: 194–201.
Mochel F, Durant B, Meng X, O'Callaghan J, Yu H, Brouillet E et al. Early alterations of brain cellular energy homeostasis in Huntington disease models. J Biol Chem 2012; 287: 1361–1370.
Drose S, Brandt U . Molecular mechanisms of superoxide production by the mitochondrial respiratory chain. Adv Exp Med Biol 2012; 748: 145–169.
Dean OM, Bush AI, Berk M . Translating the Rosetta Stone of N-acetylcysteine. Biol Psychiatry 2012; 71: 935–936.
Acknowledgements
We thank Peter Crouch for his insightful feedback and the Australian Mitochondrial Disease Foundation for partial support of purchasing the Seahorse XF24 Extracellular Flux Analyzer. The Florey Institute of Neuroscience and Mental Health acknowledges the support from the Victorian Government’s Operational Infrastructure Support Grant. This work was supported by an Australian Research Council FT3 Future Fellowship (FT100100835) to AJH, National Health and Medical Research Council Career Development Fellowships to SLM (APP1030474) and AEF (APP541920) and a National Health and Medical Research Council Principal Research Fellowship to DRT (APP1022896). DJW holds a University of Melbourne Australian Postgraduate Award. TR is supported by an Australian Research Council Discovery Early Career Research Award (DE140100588).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Translational Psychiatry website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Wright, D., Renoir, T., Smith, Z. et al. N-Acetylcysteine improves mitochondrial function and ameliorates behavioral deficits in the R6/1 mouse model of Huntington's disease. Transl Psychiatry 5, e492 (2015). https://doi.org/10.1038/tp.2014.131
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2014.131
This article is cited by
-
New Pharmacologic Approaches to the Treatment of Bipolar Depression
Drugs (2023)
-
Quantitative Phosphoproteomics Reveals Extensive Protein Phosphorylation Dysregulation in the Cerebral Cortex of Huntington’s Disease Mice Prior to Onset of Symptoms
Molecular Neurobiology (2022)
-
Increasing Nrf2 Activity as a Treatment Approach in Neuropsychiatry
Molecular Neurobiology (2021)
-
Mitochondrial Abnormalities and Synaptic Damage in Huntington’s Disease: a Focus on Defective Mitophagy and Mitochondria-Targeted Therapeutics
Molecular Neurobiology (2021)
-
Tetrahydrobenzimidazole TMQ0153 triggers apoptosis, autophagy and necroptosis crosstalk in chronic myeloid leukemia
Cell Death & Disease (2020)