Abstract
Objectives
The objective of this study is to examine, from a limited societal perspective, the cost-effectiveness of community-based obesity prevention interventions (CBIs)-defined as a programme of community-level strategies to promote healthy eating and physical activity for Australian children (aged 5–18 years).
Methods
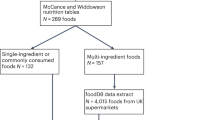
The effectiveness of CBIs was determined by undertaking a literature review and meta-analysis. Commonly implemented strategies to increase physical activity and improve nutrition were costed (in 2010 Australian dollars) to determine the average cost of a generic programme. A multiple cohort Markov model that simulates diseases associated with overweight and obesity was used to estimate the health benefits, measured as health-adjusted life years (HALYs) and healthcare-related cost offsets from diseases averted due to exposure to the intervention. Health and cost outcomes were estimated over the lifetime of the target population. Monte-Carlo simulation was used to assess second-order uncertainty of input parameters to estimate mean incremental cost-effectiveness ratios (ICER) with 95% uncertainty intervals (UIs). Scenario analyses tested variations in programme intensity, target population, and duration of effect.
Results
The meta-analysis revealed a small but significant difference in BMI z-score (mean difference of − 0.07 (95% UI: − 0.13 to − 0.01)) favouring the CBI community compared with the control. The estimated net cost of implementing CBIs across all local government areas (LGAs) in Australia was AUD426M (95% UI: AUD3M to AUD823M) over 3 years. This resulted in 51,792 HALYs gained (95% UI: 6816 to 96,972) over the lifetime of the cohort. The mean ICER was AUD8155 per HALY gained (95% UI: AUD237 to AUD81,021), with a 95% probability of being cost-effective at a willingness to pay threshold of AUD50,000 per HALY.
Conclusions
CBIs are cost-effective obesity prevention initiatives; however, implementation across Australia will be (relatively) expensive when compared with current investments in preventive health.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128· 9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Australian Institute of Health and Welfare. Australia’s health 2016. Canberra: AIHW; 2016.
Duckett S, Swerissen H, Wiltshire T. A sugary drinks tax: recovering the community costs of obesity. Melbourne: Grattan Institute; 2016.
Colagiuri S, Lee CM, Colagiuri R, Magliano D, Shaw JE, Zimmet PZ, et al. The cost of overweight and obesity in Australia. Med J Aust. 2010;192:260–4.
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–14.
Wolfenden L, Wyse R, Nichols M, Allender S, Millar L, McElduff P. A systematic review and meta-analysis of whole of community interventions to prevent excessive population weight gain. Prev Med. 2014;62:193–200.
Waters E, Silva-Sanigorski Ad, Burford BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;12:128–9.
Swinburn B, Malakellis M, Moodie M, Waters E, Gibbs L, Millar L, et al. Large reductions in child overweight and obesity in intervention and comparison communities 3 years after a community project. Pediatr Obes. 2014;9:455–62.
Rush E, McLennan S, Obolonkin V, Vandal AC, Hamlin M, Simmons D, et al. Project Energize: whole-region primary school nutrition and physical activity programme; evaluation of body size and fitness 5 years after the randomised controlled trial. Br J Nutr. 2014;111:363–71.
Borys JM, Le Bodo Y, Jebb SA, Seidell J, Summerbell C, Richard D, et al. EPODE approach for childhood obesity prevention: methods, progress and international development. Obes Rev. 2012;13:299–315.
Romon M, Lommez A, Tafflet M, Basdevant A, Oppert JM, Bresson JL, et al. Downward trends in the prevalence of childhood overweight in the setting of 12-year school-and community-based programmes. Public Health Nutr. 2009;12:1735–42.
Flego A, Keating C, Moodie M. Cost–effectiveness of whole-of-community obesity prevention programs: an overview of the evidence. Expert Rev Pharm Outcomes Res. 2015;14:719–27.
Bleich SN, Segal J, Wu Y, Wilson R, Wang Y. Systematic review of community-based childhood obesity prevention studies. Pediatrics. 2013;132:p201–10.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
EPHPP. Quality assessment tool for quantitative studies: Effective Public Health Practice Project 2010 [Available from: http://www.ephpp.ca/PDF/Quality%20Assessment%20Tool_2010_2.pdf].
Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95:89–98.
Borys J, Valdeyron L, Levy E, Vinck J, Edell D, Walter L, et al. EPODE a model for reducing the incidence of obesity and weight-related comorbidities. Endocrinology. 2013;9:32–6.
Brown V, Moodie M, Cobiac L, Herrera AM, Carter R. Obesity-related health impacts of fuel excise taxation-an evidence review and cost-effectiveness study. BMC Public Health. 2017;17:359.
Lal A, Mantilla-Herrera AM, Veerman L, Backholer K, Sacks G, Moodie M, et al. Modelled health benefits of a sugar-sweetened beverage tax across different socioeconomic groups in Australia: a cost-effectiveness and equity analysis. PLoS Med. 2017;14:e1002326.
Crino M, Herrera AMM, Ananthapavan J, Wu JH, Neal B, Lee YY, et al. Modelled cost-effectiveness of a package size cap and a kilojoule reduction intervention to reduce energy intake from sugar-sweetened beverages in Australia. Nutrients. 2017;9:983.
Brown V, Ananthapavan J, Veerman L, Sacks G, Lal A, Peeters A, et al. The potential cost-effectiveness and equity impacts of restricting television advertising of unhealthy food and beverages to Australian children. Nutrients. 2018;10:622.
Mantilla Herrera A, Crino M, Erskine H, Sacks G, Ananthapavan J, Mhurchu C, et al. Cost-effectiveness of product reformulation in response to the health star rating food labelling system in Australia. Nutrients. 2018;10:614.
Barendregt JJ, Veerman JL. Categorical versus continuous risk factors and the calculation of potential impact fractions. J Epidemiol Community Health. 2010;64:209–12.
Murray CJ, Abraham J, Ali MK, Alvarado M, Atkinson C, Baddour LM, et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–606.
Global Burden of Disease Study 2010 (GBD 2010). Results by risk factor 1990–2010 [Internet]. Institute for Health Metrics and Evaluation (IHME); 2012. Available from: http://www.healthdata.org.
Australian Bureau of Statistics. 2011 Census of population and housing. Canberra: Australian Bureau of Statistics; 2012.
Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380:2129–43.
Chen G, Ratcliffe J, Olds T, Magarey A, Jones M, Leslie E. BMI, health behaviors, and quality of life in children and adolescents: a school-based study. Pediatrics. 2014;133:e868–e74.
Moodie ML, Herbert JK, Silva-Sanigorski AMd, Mavoa HM, Keating CL, Carter RC, et al. The cost-effectiveness of a successful community-based obesity prevention program: the be active eat well program. Obesity. 2013;21:2072–80.
Sanigorski AM, Bell A, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity-building: results of a quasi-experimental intervention program, Be Active Eat Well. Int J Obes. 2008;32:1060–67.
Sanigorski A, Prosser L, Carpenter L, Honisett S, Gibbs L, Moodie M, et al. Evaluation of the childhood obesity prevention program Kids– ‘Go for your life’. BMC Public Health. 2010;10:288.
Salmon J, Arundell L, Hume C, Brown H, Hesketh K, Dunstan DW, et al. A cluster-randomized controlled trial to reduce sedentary behavior and promote physical activity and health of 8-9 year olds: The Transform-Us! Study. BMC Public Health. 2011;11:759.
Rush E, Obolonkin V, McLennan S, Graham D, Harris JD, Mernagh P, et al. Lifetime cost effectiveness of a through-school nutrition and physical programme: project Energize. Obes Res Clin Pract. 2014;8:e115–e22.
McAuley KA, Taylor RW, Farmer VL, Hansen P, Williams SM, Booker CS, et al. Economic evaluation of a community-based obesity prevention program in children: the APPLE project. Obesity (Silver Spring, MD). 2010;18:131–6.
Australian Bureau of Statistics. 6348.0 - Labour costs, Australia, 2010–11. Canberra: ABS; 2012.
Australian Bureau of Statistics. 63060DO001_201005 Employee earnings and hours, Australia, May 2010. Canberra: ABS; 2011.
Australian Bureau of Statistics. 63060DO011_201405 Employee earnings and hours, Australia, May 2014. Canberra: Australian Bureau of Statistics; 2015.
Cadilhac D, Magnus A, Cumming T, Sheppard L, Pearce D, Carter R. The health and economic benefits of reducing disease risk factors. Melbourne: VicHealth; 2009.
Australian Bureau of Statistics. 6302.0 - Average weekly earnings Australia. Canberra: ABS; 2010.
Australian Institute of Health and Welfare. Health system expenditure on disease and injury in Australia, 2000–01. Canberra: AIHW; 2004.
Australian Institute of Health and Welfare. Health expenditure Australia 2014–15. Canberra: AIHW; 2016.
Gold M, Siegel J, Russell L, Weinstein M. Cost-effectiveness in health and medicine. New York: Oxford Univ. Press; 1996.
Stinnett AA, Paltiel AD. Estimating CE ratios under second-order uncertainty: the mean ratio versus the ratio of means. Med Decis Mak. 1997;17:483–9.
George B, Harris A, Mitchell A. Cost-effectiveness analysis and the consistency of decision making: evidence from pharmaceutical reimbursement in Australia (1991 to 1996). Pharmacoeconomics. 2001;19:1103–9.
Whelan J, Love P, Pettman T, Doyle J, Booth S, Smith E, et al. Cochrane update: predicting sustainability of intervention effects in public health evidence: identifying key elements to provide guidance. J Public Health (Bangk). 2014;36:347–51.
De Coen V, De Bourdeaudhuij I, Vereecken C, Verbestel V, Haerens L, Huybrechts I, et al. Effects of a 2-year healthy eating and physical activity intervention for 3-6-year-olds in communities of high and low socio-economic status: the POP (Prevention of Overweight among Pre-school and school children) project. Public Health Nutr. 2012;15:1737–45.
De Henauw S, Huybrechts I, De Bourdeaudhuij I, Bammann K, Barba G, Lissner L, et al. Effects of a community-oriented obesity prevention programme on indicators of body fatness in preschool and primary school children. Main results from the IDEFICS study. Obes Rev. 2015;16:16–29.
Economos CD, Hyatt RR, Must A, Goldberg JP, Kuder J, Naumova EN, et al. Shape Up Somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Prev Med. 2013;57:322–7.
Taylor RW, McAuley KA, Barbezat W, Strong A, Williams SM, Mann JI. APPLE Project: 2-y findings of a community-based obesity prevention program in primary school–age children. Am J Clin Nutr. 2007;86:735–42.
Utter J, Scragg R, Robinson E, Warbrick J, Faeamani G, Foroughian S, et al. Evaluation of the Living 4 Life project: a youth‐led, school‐based obesity prevention study. Obes Rev. 2011;12(s2):51–60.
Millar L, Kremer P, de Silva‐Sanigorski A, McCabe M, Mavoa H, Moodie M, et al. Reduction in overweight and obesity from a 3‐year community‐based intervention in Australia: the ‘It’s Your Move!’project. Obes Rev. 2011;12(s2):20–8.
Fotu KF, Millar L, Mavoa H, Kremer P, Moodie M, Snowdon W, et al. Outcome results for the Ma’alahi Youth Project, a Tongan community-based obesity prevention programme for adolescents. Obes Rev. 2011;12:41–50.
Kremer P, Waqa G, Vanualailai N, Schultz J, Roberts G, Moodie M, et al. Reducing unhealthy weight gain in Fijian adolescents: results of the Healthy Youth Healthy Communities study. Obes Rev. 2011;12(s2):29–40.
Silva-Sanigorski AM, Bell AC, Kremer P, Nichols M, Crellin M, Smith M, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr. 2010;91:831–40.
Australian Bureau of Statistics. Schools, Australia (cat. no. 4221.0). Canberra: ABS; 2011.
Hillier-Brown FC, Bambra CL, Cairns J-M, Kasim A, Moore HJ, Summerbell CD. A systematic review of the effectiveness of individual, community and societal level interventions at reducing socioeconomic inequalities in obesity amongst children. BMC Public Health. 2014;14:834.
Bolton KA, Kremer P, Gibbs L, Swinburn B, Waters E, de Silva A. Expanding a successful community-based obesity prevention approach into new communities: Challenges and achievements. Obes Res Clin Pract. 2016;10:197–206.
Council of Australian Governments. National partnership agreement on preventive health. Canberra: COAG; 2009.
Sweeney R, Moodie M, Nguyen P, Fraser P, Bolton K, Brown A, et al. Protocol for an economic evaluation of WHO STOPS childhood obesity stepped-wedge cluster randomised controlled trial. BMJ Open. 2018;8:e020551.
World Health Organization. Population-based approaches to childhood obesity prevention. Geneva: WHO; 2012.
Acknowledgements
The authors acknowledge the contribution of data from Dr Luke Wolfenden.
Funding source
The work was funded by a National Health and Medical Research Council (NHMRC) Centre of Research Excellence (CRE) on Obesity Policy and Food Systems (Grant number 1041020). GS is the recipient of an Australian Research Council Discovery Early Career Researcher Award (DE160100307).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ananthapavan, J., Nguyen, P.K., Bowe, S.J. et al. Cost-effectiveness of community-based childhood obesity prevention interventions in Australia. Int J Obes 43, 1102–1112 (2019). https://doi.org/10.1038/s41366-019-0341-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0341-0
This article is cited by
-
Are climate-change actions present in community-based obesity prevention interventions? Development and application of the DoublE-duty actions in CommunIty-baSed obesity InterVEntions (DECISIVE) framework
Journal of Public Health (2024)
-
Primary prevention programs for childhood obesity: are they cost-effective?
Italian Journal of Pediatrics (2023)
-
Economic evaluation of an incentive-based program to increase physical activity and reduce sedentary behaviour in middle-aged adults
BMC Health Services Research (2022)
-
A cost–benefit analysis framework for preventive health interventions to aid decision-making in Australian governments
Health Research Policy and Systems (2021)
-
Stakeholders perspectives of barriers and facilitators of childhood obesity prevention policies in Iran: A Delphi method study
BMC Public Health (2021)