Abstract
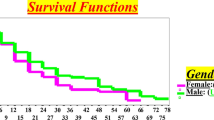
Manifestations of viral infections can differ between women and men1, and marked sex differences have been described in the course of HIV-1 disease. HIV-1–infected women tend to have lower viral loads early in HIV-1 infection but progress faster to AIDS for a given viral load than men2,3,4,5,6,7. Here we show substantial sex differences in the response of plasmacytoid dendritic cells (pDCs) to HIV-1. pDCs derived from women produce markedly more interferon-α (IFN-α) in response to HIV-1–encoded Toll-like receptor 7 (TLR7) ligands than pDCs derived from men, resulting in stronger secondary activation of CD8+ T cells. In line with these in vitro studies, treatment-naive women chronically infected with HIV-1 had considerably higher levels of CD8+ T cell activation than men after adjusting for viral load. These data show that sex differences in TLR-mediated activation of pDCs may account for higher immune activation in women compared to men at a given HIV-1 viral load and provide a mechanism by which the same level of viral replication might result in faster HIV-1 disease progression in women compared to men. Modulation of the TLR7 pathway in pDCs may therefore represent a new approach to reduce HIV-1–associated pathology.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Fish, E.N. The X-files in immunity: sex-based differences predispose immune responses. Nat. Rev. Immunol. 8, 737–744 (2008).
Katzenstein, D.A. et al. The relation of virologic and immunologic markers to clinical outcomes after nucleoside therapy in HIV-infected adults with 200 to 500 CD4 cells per cubic millimeter. AIDS Clinical Trials Group Study 175 Virology Study Team. N. Engl. J. Med. 335, 1091–1098 (1996).
Farzadegan, H. et al. Sex differences in HIV-1 viral load and progression to AIDS. Lancet. 352, 1510–1514 (1998).
Evans, J.S. et al. Serum levels of virus burden in early-stage human immunodeficiency virus type 1 disease in women. J. Infect. Dis. 175, 795–800 (1997).
Sterling, T.R. et al. Sex differences in longitudinal human immunodeficiency virus type 1 RNA levels among seroconverters. J. Infect. Dis. 180, 666–672 (1999).
Lyles, C.M. et al. Longitudinal human immunodeficiency virus type 1 load in the Italian seroconversion study: correlates and temporal trends of virus load. J. Infect. Dis. 180, 1018–1024 (1999).
Gandhi, M. et al. Does patient sex affect human immunodeficiency virus levels? Clin. Infect. Dis. 35, 313–322 (2002).
Fahey, J.L. et al. The prognostic value of cellular and serologic markers in infection with human immunodeficiency virus type 1. N. Engl. J. Med. 322, 166–172 (1990).
Fahey, J.L. et al. Prognostic significance of plasma markers of immune activation, HIV viral load and CD4 T-cell measurements. AIDS 12, 1581–1590 (1998).
Giorgi, J.V. et al. Shorter survival in advanced human immunodeficiency virus type 1 infection is more closely associated with T lymphocyte activation than with plasma virus burden or virus chemokine coreceptor usage. J. Infect. Dis. 179, 859–870 (1999).
Deeks, S.G. & Walker, B.D. The immune response to AIDS virus infection: good, bad or both? J. Clin. Invest. 113, 808–810 (2004).
Deeks, S.G. et al. Immune activation set point during early HIV infection predicts subsequent CD4+ T-cell changes independent of viral load. Blood 104, 942–947 (2004).
Hunt, P.W. et al. Relationship between T cell activation and CD4+ T cell count in HIV-seropositive individuals with undetectable plasma HIV RNA levels in the absence of therapy. J. Infect. Dis. 197, 126–133 (2008).
Sousa, A.E., Carneiro, J., Meier-Schellersheim, M., Grossman, Z. & Victorino, R.M. CD4 T cell depletion is linked directly to immune activation in the pathogenesis of HIV-1 and HIV-2 but only indirectly to the viral load. J. Immunol. 169, 3400–3406 (2002).
Silvestri, G. et al. Nonpathogenic SIV infection of sooty mangabeys is characterized by limited bystander immunopathology despite chronic high-level viremia. Immunity 18, 441–452 (2003).
Boasso, A. & Shearer, G.M. Chronic innate immune activation as a cause of HIV-1 immunopathogenesis. Clin. Immunol. 126, 235–242 (2008).
Beignon, A.S. et al. Endocytosis of HIV-1 activates plasmacytoid dendritic cells via Toll-like receptor–viral RNA interactions. J. Clin. Invest. 115, 3265–3275 (2005).
Chang, J.J. & Altfeld, M. TLR-mediated immune activation in HIV. Blood 113, 269–270 (2009).
Heil, F. et al. Species-specific recognition of single-stranded RNA via Toll-like receptor 7 and 8. Science 303, 1526–1529 (2004).
Meier, A. et al. MyD88-dependent immune activation mediated by HIV-1-encoded TLR ligands. J. Virol. 81, 8180–8191 (2007).
Berghöfer, B. et al. TLR7 ligands induce higher IFN-α production in females. J. Immunol. 177, 2088–2096 (2006).
Hughes, G.C., Thomas, S., Li, C., Kaja, M.K. & Clark, E.A. Cutting edge: progesterone regulates IFN-α production by plasmacytoid dendritic cells. J. Immunol. 180, 2029–2033 (2008).
Eyster, M.E., Goedert, J.J., Poon, M.C. & Preble, O.T. Acid-labile α interferon. A possible preclinical marker for the acquired immunodeficiency syndrome in hemophilia. N. Engl. J. Med. 309, 583–586 (1983).
Krown, S.E. et al. Relationship and prognostic value of endogenous interferon-α, β2-microglobulin and neopterin serum levels in patients with Kaposi sarcoma and AIDS. J. Acquir. Immune Defic. Syndr. 4, 871–880 (1991).
Mildvan, D., Machado, S.G., Wilets, I. & Grossberg, S.E. Endogenous interferon and triglyceride concentrations to assess response to zidovudine in AIDS and advanced AIDS-related complex. Lancet 339, 453–456 (1992).
Rodriguez, B. et al. Interferon-α differentially rescues CD4 and CD8 T cells from apoptosis in HIV infection. AIDS 20, 1379–1389 (2006).
Gandhi, R.T. et al. Effect of baseline- and treatment-related factors on immunologic recovery after initiation of antiretroviral therapy in HIV-1–positive subjects: results from ACTG 384. J. Acquir. Immune Defic. Syndr. 42, 426–434 (2006).
Robbins, G.K. et al. Comparison of sequential three-drug regimens as initial therapy for HIV-1 infection. N. Engl. J. Med. 349, 2293–2303 (2003).
Sterling, T.R. et al. Initial plasma HIV-1 RNA levels and progression to AIDS in women and men. N. Engl. J. Med. 344, 720–725 (2001).
Giorgi, J.V. et al. Elevated levels of CD38+ CD8+ T cells in HIV infection add to the prognostic value of low CD4+ T cell levels: results of 6 years of follow-up. The Los Angeles Center, Multicenter AIDS Cohort Study. J. Acquir. Immune Defic. Syndr. 6, 904–912 (1993).
Liu, Z. et al. Elevated CD38 antigen expression on CD8+ T cells is a stronger marker for the risk of chronic HIV disease progression to AIDS and death in the Multicenter AIDS Cohort Study than CD4+ cell count, soluble immune activation markers, or combinations of HLA-DR and CD38 expression. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 16, 83–92 (1997).
Boasso, A., Hardy, A.W., Anderson, S.A., Dolan, M.J. & Shearer, G.M. HIV-induced type I interferon and tryptophan catabolism drive T cell dysfunction despite phenotypic activation. PLoS One 3, e2961 (2008).
Herbeuval, J.P. et al. Differential expression of IFN-α and TRAIL/DR5 in lymphoid tissue of progressor versus nonprogressor HIV-1–infected patients. Proc. Natl. Acad. Sci. USA 103, 7000–7005 (2006).
Herbeuval, J.P. & Shearer, G.M. HIV-1 immunopathogenesis: how good interferon turns bad. Clin. Immunol. 123, 121–128 (2007).
Mandl, J.N. et al. Divergent TLR7 and TLR9 signaling and type I interferon production distinguish pathogenic and nonpathogenic AIDS virus infections. Nat. Med. 14, 1077–1087 (2008).
Khatissian, E., Chakrabarti, L. & Hurtrel, B. Cytokine patterns and viral load in lymph nodes during the early stages of SIV infection. Res. Virol. 147, 181–189 (1996).
Silvestri, G., Paiardini, M., Pandrea, I., Lederman, M.M. & Sodora, D.L. Understanding the benign nature of SIV infection in natural hosts. J. Clin. Invest. 117, 3148–3154 (2007).
Barrat, F.J. et al. Nucleic acids of mammalian origin can act as endogenous ligands for Toll-like receptors and may promote systemic lupus erythematosus. J. Exp. Med. 202, 1131–1139 (2005).
Guiducci, C., Coffman, R.L. & Barrat, F.J. Signalling pathways leading to IFN-α production in human plasmacytoid dendritic cell and the possible use of agonists or antagonists of TLR7 and TLR9 in clinical indications. J. Intern. Med. 265, 43–57 (2009).
Acknowledgements
We thank S. Deeks, P. Hunt, B. Walker and J. Spritzler for valuable intellectual input and discussions and the ACTG 384 main study and immunology A5007 substudy teams. These studies were supported by US National Institutes of Health (NIH)–National Institute of Allergy and Infectious Diseases grants to M.A. (R21 AI071806, PO1 AI074415) and G.K.R. (K01AI062435), the Harvard University Center for AIDS Research, the Bill & Melinda Gates Foundation and the Doris Duke Charitable Foundation. A.M. was supported by a fellowship from the German Research Society (Deutsche Forschungsgemeinschaft), and J.J.C. was supported by a Fellowship awarded from the National Health and Medical Research Council of Australia (519578). ACTG 384 was supported in part by National Institute of Allergy and Infectious Diseases grants AI38855, AI27659, AI38858, AI25879 and AI27666 and by Agouron/Pfizer, Bristol Myers Squibb and GlaxoSmithKline. This project has been funded in whole or in part with federal funds from the US National Cancer Institute (NCI), NIH, under Contract number HHSN261200800001E. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does the mention of trade names, commercial products or organizations imply endorsement by the US Government. This research was supported in part by the Intramural Research Support Program of the NIH, NCI, Center for Cancer Research. M.A. is a Distinguished Clinical Scientist of the Doris Duke Charitable Foundation. We thank the Mark and Lisa Schwartz Foundation and the Phillip T. and Susan M. Ragon Foundation for their support.
Author information
Authors and Affiliations
Contributions
A.M. and J.J.C. conducted the in vitro experiments, data analysis and contributed to manuscript preparation; H.K.S., T.F.W. and R.J.L. also conducted the in vitro experiments; E.S.C., R.J.B., L.O. and D.M. contributed to the statistical analysis and interpretation of the data; A.M., J.J.C., R.J.B., G.A., H.S. and M.A. participated in the planning of the experiments; S.K. and M.C. conducted the genetic polymorphism experiments; S.B. helped with the enrollment of study subjects, R.B.P. and G.K.R. provided the data for ACTG 384; J.D.L. provided the AT-2 virus and vesicle controls used in the in vitro experiments; and M.A. planned the studies, prepared the manuscript and supervised the project.
Corresponding author
Supplementary information
Supplementary Text and Figures
Supplementary Table 1 (PDF 196 kb)
Rights and permissions
About this article
Cite this article
Meier, A., Chang, J., Chan, E. et al. Sex differences in the Toll-like receptor–mediated response of plasmacytoid dendritic cells to HIV-1. Nat Med 15, 955–959 (2009). https://doi.org/10.1038/nm.2004
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.2004
This article is cited by
-
Mechanisms and consequences of sex differences in immune responses
Nature Reviews Nephrology (2024)
-
Proteins in pregnant swine serum promote the African swine fever virus replication: an iTRAQ-based quantitative proteomic analysis
Virology Journal (2023)
-
Sex differences in the percentage of IRF5 positive B cells are associated with higher production of TNF-α in women in response to TLR9 in humans
Biology of Sex Differences (2023)
-
Sex, gender and infectious disease
Nature Microbiology (2022)
-
Greater Sensorimotor Deficits and Abnormally Lower Globus Pallidus Fractional Anisotropy in HIV+ Women than in HIV+ Men
Journal of Neuroimmune Pharmacology (2021)