Abstract
Background/Objectives:
Thoracic radiotherapy (RT) is associated with acute toxicities, including oesophagitis, which can have an impact on nutritional intake and subsequently lead to malnutrition. This study aimed to identify RT dosimetric factors associated with ⩾5% weight loss in patients receiving treatment for non-small-cell lung cancer (NSCLC).
Methods:
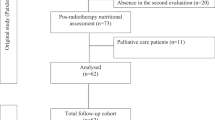
Radiation dose data to the oesophagus (including mean, maximum dose and oesophageal length) were retrospectively analysed for a cohort of 54 NSCLC patients treated with concurrent chemoradiotherapy between 2004 and 2006. Weight change was calculated using the lowest weight during the 90 days from RT commencement compared with the start of RT.
Results:
Four patients for whom weight was not available at the start or end of treatment were excluded, leaving 50 patients for analysis. The prevalence of significant weight loss during the 90 days from RT commencement was 22% (median weight loss=9.1%, range=5.9–22.1). Dosimetric factors significantly associated with ⩾5% weight loss were maximum dose to the oesophagus (P=0.046), absolute oesophageal length receiving 40 Gy (odds ratio (OR)=1.18, P=0.04), 50 Gy (OR=1.20, P=0.02) and 60 Gy (OR=1.32, P=0.005) to the partial circumference, relative oesophageal length receiving 50 Gy (OR=1.03, P=0.03) and 60 Gy (OR=1.07, P=0.005) to the partial circumference.
Conclusions:
Multiple dosimetric factors were associated with significant weight loss. Of these factors, absolute and relative length of the oesophagus receiving 60 Gy to the partial circumference were more strongly related. Understanding the dosimetric factors associated with weight loss may aid early identification and intervention in patients at nutritional risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Rose J, Rodrigues G, Yaremko B, Lock M, D' Souza D . Systematic review of dose–volume parameters in the prediction of esophagitis in thoracic radiotherapy. Radiother Oncol 2009; 91: 282–287.
Lehman M . What is the recommended treatment approach for the definitive management of patients with good performance status and inoperable stage III disease? In: Cancer Council Australia Lung Cancer Guidelines Working Party: Clinical practice guidelines for the treatment of lung cancer. Cancer Council Australia: Sydney, 2012. Accessed on 21 October 2013 at http://wiki.cancer.org.au/australia/Guidelines:Lung_cancer).
Byhardt RW, Scott C, Sause WT, Emami B, Komaki R, Fisher B et al. Response, toxicity, failure patterns, and survival in five radiation therapy oncology group (RTOG) trials of sequential and/or concurrent chemotherapy and radiotherapy for locally advanced non–small-cell carcinoma of the lung. Int J Radiat Oncol Biol Phys 1998; 42: 469–478.
Bovio G, Montagna G, Bariani C, Baiardi P . Upper gastrointestinal symptoms in patients with advanced cancer: relationship to nutritional and performance status. Support Care Cancer 2009; 17: 1317–1324.
Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Am J Med 1980; 69: 491–497.
Ross PJ, Ashley S, Norton A, Priest K, Waters JS, Eisen T et al. Do patients with weight loss have a worse outcome when undergoing chemotherapy for lung cancers? Br J Cancer 2004; 90: 1905–1911.
Hill A, Kiss N, Hodgson B, Crowe TC, Walsh AD . Associations between nutritional status, weight loss, radiotherapy treatment toxicity and treatment outcomes in gastrointestinal cancer patients. Clin Nutr 2011; 30: 92–98.
Jager-Wittenaar H, Dijkstra PU, Vissink A, van der Laan B, van Oort RP, Roodenburg JLN . Malnutrition and quality of life in patients treated for oral or oropharyngeal cancer. Head Neck 2011; 33: 490–496.
Norman K, Stobaus N, Smoliner C, Zocher D, Scheufele R, Valentini L et al. Determinants of hand grip strength, knee extension strength and functional status in cancer patients. Clin Nutr 2010; 29: 586–591.
Capuano G, Grosso A, Gentile PC, Battista M, Bianciardi F, Di Palma A et al. Influence of weight loss on outcomes in patients with head and neck cancer undergoing concomitant chemoradiotherapy. Head Neck 2008; 30: 503–508.
Buskermolen S, Langius JAE, Kruizenga HM, Ligthart-Melis GC, Heymans MW, Verheul HM . Weight Loss of 5% or more predicts loss of fat-free mass during palliative chemotherapy in patients with advanced cancer: a pilot study. Nutr Cancer 2012; 64: 826–832.
Findlay M, Bauer J, Brown T, Davidson W, Hill J, Isenring E et al. Evidence Based Practice Guidelines for the Nutritional Managment of Adult Patients with Head and Neck Cancer. Clinical Oncology Society of Australia: Sydney, 2011 Accessed on 20 April 2013 at http://wiki.cancer.org.au/australia/COSA:Head_and_neck_cancer_nutrition_guidelines).
Cartmill B, Cornwell P, Ward E, Davidson W, Nund R, Bettington C et al. Emerging understanding of dosimetric factors impacting on dysphagia and nutrition following radiotherapy for oropharyngeal cancer. Head Neck 2013; 35: 1211–1219.
Gardine RL, Kokal WA, Beatty JD, Riihimaki DU, Wagman LD, Terz JJ . Predicting the need for prolonged enteral supplementation in the patient with head and neck cancer. Am J Surg 1988; 156: 63–65.
Gokhale AS, McLaughlin BT, Flickinger JC, Beriwal S, Heron DE, Ferris RL et al. Clinical and dosimetric factors associated with a prolonged feeding tube requirement in patients treated with chemoradiotherapy (CRT) for head and neck cancers. Ann Oncol 2010; 21: 145–151.
Poulsen MG, Riddle B, Keller J, Porceddu SV, Tripcony L . Predictors of acute grade 4 swallowing toxicity in patients with stages III and IV squamous carcinoma of the head and neck treated with radiotherapy alone. Radiother Oncol 2008; 87: 253–259.
Bradley J, Deasy JO, Bentzen S, El Naqa I . Dosimetric correlates for acute esophagitis in patients treated with radiotherapy for lung carcinoma. Int J Radiat Oncol Biol Phys 2004; 58: 1106–1113.
Maguire PD, Sibley GS, Zhou S-M, Jamieson TA, Light KL, Antione PA et al. Clinical and dosimetric predictors of radiation-induced esophageal toxicity. Int J Radiat Oncol Biol Phys 1999; 45: 97–103.
Singh AK, Lockett MA, Bradley JD . Predictors of radiation-induced esophageal toxicity in patients with non-small-cell lung cancer treated with three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys 2003; 55: 337–341.
Ottery F . Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition 12: S15–S19 1996.
National Cancer Institute: Common Terminology Criteria for Adverse Events v3.0. US Department of Health and Human Services, National Institute of Health. National Cancer Institute, 2003.
Caudell JJ, Schaner PE, Desmond RA, Meredith RF, Spencer SA, Bonner JA . Dosimetric factors associated with long-term dysphagia after definitive radiotherapy for squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys 2010; 76: 403–409.
Mariani L, Lo Vullo S, Bozzetti F . Weight loss in cancer patients: a plea for a better awareness of the issue. Support Care Cancer 2012; 20: 301–309.
Palma DA, Senan S, Oberije C, Belderbos J, Dios NR, Bradley JD et al. Predicting esophagitis after chemoradiation therapy for non-small cell lung cancer: an individual patient data meta-analysis. Int J Radiat Oncol Biol Phys 2013; 87: 690–696.
Hirota S, Tsujino K, Endo M, Kotani Y, Satouchi M, Kado T et al. Dosimetric predictors of radiation esophagitis in patients treated for non-small-cell lung cancer with carboplatin/paclitaxel/radiotherapy. Int J Radiat Oncol Biol Phys 2001; 51: 291–295.
Huang EX, Bradley JD, El Naqa I, Hope AJ, Lindsay PE, Bosch WR et al. Modeling the Risk of Radiation-Induced Acute Esophagitis for Combined Washington University and RTOG Trial 93-11 Lung Cancer Patients. Int J Radiat Oncol Biol Phys 2012; 82: 1674–1679.
Kiss N, Isenring E, Gough K, Krishnasamy M . The prevalence of weight loss during (chemo)radiotherapy treatment for lung cancer and associated patient- and treatment-related factors. Clinical Nutrition 2013; e-pub ahead of print 27 November 2013; doi:10.1016/j.clnu.2013.11.013.
Bezjak A, Rumble RB, Rodrigues G, Hope A, Warde P . Intensity-modulated radiotherapy in the treatment of lung cancer. Clin Oncol 2012; 24: 508–520.
Isenring E, Zabel R, Bannister M, Brown T, Findlay M, Kiss N et al. Updated evidence-based practice guidelines for the nutritional management of patients receiving radiation therapy and/or chemotherapy. Nutr Diet 2013; 70: 312–324.
Brown TE, Spurgin A-L, Ross L, Tripcony L, Keller J, Hughes BGM et al. Validated swallowing and nutrition guidelines for patients with head and neck cancer: Identification of high-risk patients for proactive gastrostomy. Head Neck 2013; 35: 1385–1391.
Kiss N, Krishnasamy M, Loeliger J, Granados A, Dutu G, Corry J . A dietitian-led clinic for patients receiving (chemo)radiotherapy for head and neck cancer. Support Care Cancer 2012; 20: 2111–2120.
Arends J, Bodoky G, Bozzetti F, Fearon K, Muscaritoli M, Selga G et al. ESPEN guidelines on enteral nutrition: non-surgical oncology. Clin Nutr 2006; 25: 249–259.
Acknowledgements
We acknowledge the contributions of D Ball, M Bressel and C Russell in the design and collection of data for the original study. This study was supported by a PhD scholarship from the Victorian Cancer Agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Kiss, N., Krishnasamy, M., Everitt, S. et al. Dosimetric factors associated with weight loss during (chemo)radiotherapy treatment for lung cancer. Eur J Clin Nutr 68, 1309–1314 (2014). https://doi.org/10.1038/ejcn.2014.166
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.166
This article is cited by
-
The Role of Malnutrition and Muscle Wasting in Advanced Lung Cancer
Current Oncology Reports (2020)