Abstract
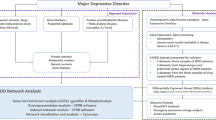
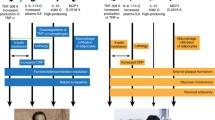
Meta-analyses confirm that depression is accompanied by signs of inflammation including increased levels of acute phase proteins, e.g., C-reactive protein, and pro-inflammatory cytokines, e.g., interleukin-6. Supporting the translational significance of this, a meta-analysis showed that anti-inflammatory drugs may have antidepressant effects. Here, we argue that inflammation and depression research needs to get onto a new track. Firstly, the choice of inflammatory biomarkers in depression research was often too selective and did not consider the broader pathways. Secondly, although mild inflammatory responses are present in depression, other immune-related pathways cannot be disregarded as new drug targets, e.g., activation of cell-mediated immunity, oxidative and nitrosative stress (O&NS) pathways, autoimmune responses, bacterial translocation, and activation of the toll-like receptor and neuroprogressive pathways. Thirdly, anti-inflammatory treatments are sometimes used without full understanding of their effects on the broader pathways underpinning depression. Since many of the activated immune-inflammatory pathways in depression actually confer protection against an overzealous inflammatory response, targeting these pathways may result in unpredictable and unwanted results. Furthermore, this paper discusses the required improvements in research strategy, i.e., path and drug discovery processes, omics-based techniques, and systems biomedicine methodologies. Firstly, novel methods should be employed to examine the intracellular networks that control and modulate the immune, O&NS and neuroprogressive pathways using omics-based assays, including genomics, transcriptomics, proteomics, metabolomics, epigenomics, immunoproteomics and metagenomics. Secondly, systems biomedicine analyses are essential to unravel the complex interactions between these cellular networks, pathways, and the multifactorial trigger factors and to delineate new drug targets in the cellular networks or pathways. Drug discovery processes should delineate new drugs targeting the intracellular networks and immune-related pathways.
Similar content being viewed by others
References
Kirsch I (2009) Antidepressants and the placebo response. Epidemiol Psychiatr Soc 18(4):318–322
Maes M (1993) A review on the acute phase response in major depression. Rev Neurosci 4(4):407–416
Berk M, Williams LJ, Jacka FN, O’Neil A, Pasco JA, Moylan S, Allen NB, Stuart AL, Hayley AC, Byrne ML, Maes M (2013) So depression is an inflammatory disease, but where does the inflammation come from? BMC Med 11:200
Fond G, Hamdani N, Kapczinski F, Boukouaci W, Drancourt N, Dargel A, Oliveira J, Le Guen E, Marlinge E, Tamouza R, Leboyer M (2014) Effectiveness and tolerance of anti-inflammatory drugs’ add-on therapy in major mental disorders: a systematic qualitative review. Acta Psychiatr Scand 129(3):163–179
Köhler O, Benros ME, Nordentoft M, Farkouh ME, Iyengar RL, Mors O, Krogh J (2014) Effect of Anti-inflammatory Treatment on Depression, Depressive Symptoms, and Adverse Effects: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Psychiatry. doi:10.1001/jamapsychiatry.2014.1611
Maes M, Bosmans E, Suy E, Vandervorst C, DeJonckheere C, Raus J (1991) Depression-related disturbances in mitogen-induced lymphocyte responses and interleukin-1 beta and soluble interleukin-2 receptor production. Acta Psychiatr Scand 84(4):379–386
Song C, Dinan T, Leonard BE (1994) Changes in immunoglobulin, complement and acute phase protein levels in the depressed patients and normal controls. J Affect Disord 30(4):283–288
Maes M, Fišar Z, Medina M, Scapagnini G, Nowak G, Berk M (2012) New drug targets in depression: inflammatory, cell-mediated immune, oxidative and nitrosative stress, mitochondrial, antioxidant, and neuroprogressive pathways. And new drug candidates–Nrf2 activators and GSK-3 inhibitors. Inflammopharmacology 20(3):127–150
Maes M, Bosmans E, Suy E, Vandervorst C, De Jonckheere C, Raus J (1990) Immune disturbances during major depression: upregulated expression of interleukin-2 receptors. Neuropsychobiology 24(3):115–120
Peet M, Murphy B, Shay J, Horrobin D (1998) Depletion of omega-3 fatty acid levels in red blood cell membranes of depressive patients. Biol Psychiatry 43(5):315–319
Maes M, Christophe A, Delanghe J, Altamura C, Neels H, Meltzer HY (1999) Lowered omega-3 polyunsaturated fatty acids in serum phospholipids and cholesteryl esters of depressed patients. Psychiatry Res 85(3):275–291
Maes M, Galecki P, Chang YS, Berk M (2011) A review on the oxidative and nitrosative stress (O&NS) pathways in major depression and their possible contribution to the (neuro)degenerative processes in that illness. Prog Neuropsychopharmacol Biol Psychiatry 35(3):676–692
Maes M, De Vos N, Pioli R, Demedts P, Wauters A, Neels H, Christophe A (2000) Lower serum vitamin E concentrations in major depression. Another marker of lowered antioxidant defenses in that illness. J Affect Disord 58(3):241–246
Maes M, Mihaylova I, Kubera M, Leunis JC, Geffard M (2011) IgM-mediated autoimmune responses directed against multiple neoepitopes in depression: new pathways that underpin the inflammatory and neuroprogressive pathophysiology. J Affect Disord 135:414–418
Maes M, Kubera M, Leunis JC (2008) The gut-brain barrier in major depression: intestinal mucosal dysfunction with an increased translocation of LPS from gram negative enterobacteria (leaky gut) plays a role in the inflammatory pathophysiology of depression. Neuroendocrinol Lett 29(1):117–124
Lucas K, Maes M (2013) Role of the toll like receptor (TLR) radical cycle in chronic inflammation: possible treatments targeting the TLR4 pathway. Mol Neurobiol 48(1):190–204
Liu J, Buisman-Pijlman F, Hutchinson MR (2014) Toll-like receptor 4: innate immune regulator of neuroimmune and neuroendocrine interactions in stress and major depressive disorder. Front Neurosci 8:309
Hung YY, Kang HY, Huang KW, Huang TL (2014) Association between toll-like receptors expression and major depressive disorder. Psychiatry Res. doi:10.1016/j.psychres.2014.07.074
Kéri S, Szabó C, Kelemen O (2014) Expression of toll-like receptors in peripheral blood mononuclear cells and response to cognitive-behavioral therapy in major depressive disorder. Brain Behav Immun 40:235–243
Maes M, Meltzer HY, Scharpé S, Bosmans E, Suy E, De Meester I, Calabrese J, Cosyns P (1993) Relationships between lower plasma L-tryptophan levels and immune-inflammatory variables in depression. Psychiatry Res 49(2):151–165
Bonaccorso S, Meltzer H, Maes M (2000) Psychological and behavioural effects of interferons. Curr Opin Psychiatry 13:673–677
Song C, Lin A, Bonaccorso S, Heide C, Verkerk R, Kenis G, Bosmans E, Scharpe S, Whelan A, Cosyns P, de Jongh R, Maes M (1998) The inflammatory response system and the availability of plasma tryptophan in patients with primary sleep disorders and major depression. J Affect Disord 49(3):211–219
Maes M, Smith R, Christophe A, Vandoolaeghe E, Van Gastel A, Neels H, Demedts P, Wauters A, Meltzer HY (1997) Lower serum high-density lipoprotein cholesterol (HDL-C) in major depression and in depressed men with serious suicidal attempts: relationship with immune-inflammatory markers. Acta Psychiatr Scand 95(3):212–221
Kubera M, Symbirtsev A, Basta-Kaim A, Borycz J, Roman A, Papp M, Claesson M (1996) Effect of chronic treatment with imipramine on interleukin 1 and interleukin 2 production by splenocytes obtained from rats subjected to a chronic mild stress model of depression. Pol J Pharmacol 48(5):503–506
Kubera M, Obuchowicz E, Goehler L, Brzeszcz J, Maes M (2011) In animal models, psychosocial stress-induced (neuro)inflammation, apoptosis and reduced neurogenesis are associated to the onset of depression. Prog Neuropsychopharmacol Biol Psychiatry 35(3):744–759
Kubera M, Curzytek K, Duda W, Leskiewicz M, Basta-Kaim A, Budziszewska B, Roman A, Zajicova A, Holan V, Szczesny E, Lason W, Maes M (2013) A new animal model of (chronic) depression induced by repeated and intermittent lipopolysaccharide administration for 4 months. Brain Behav Immun 31:96–104
Gárate I, García-Bueno B, Madrigal JL, Bravo L, Berrocoso E, Caso JR, Micó JA, Leza JC (2011) Origin and consequences of brain Toll-like receptor 4 pathway stimulation in an experimental model of depression. J Neuroinflammation 8:151
Gárate I, Garcia-Bueno B, Madrigal JL, Caso JR, Alou L, Gomez-Lus ML, Micó JA, Leza JC (2013) Stress-induced neuroinflammation: role of the Toll-like receptor-4 pathway. Biol Psychiatry 73(1):32–43
Maes M, Yirmyia R, Noraberg J, Brene S, Hibbeln J, Perini G, Kubera M, Bob P, Lerer B, Maj M (2009) The inflammatory & neurodegenerative (I&ND) hypothesis of depression: leads for future research and new drug developments in depression. Metab Brain Dis 24(1):27–53
Berk M, Kapczinski F, Andreazza AC, Dean OM, Giorlando F, Maes M, Yücel M, Gama CS, Dodd S, Dean B, Magalhães PV, Amminger P, McGorry P, Malhi GS (2011) Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress and neurotrophic factors. Neurosci Biobehav Rev 35(3):804–817
Moylan S, Maes M, Wray NR, Berk M (2013) The neuroprogressive nature of major depressive disorder: pathways to disease evolution and resistance, and therapeutic implications. Mol Psychiatry 18(5):595–606
Catena-Dell’Osso M, Bellantuono C, Consoli G, Baroni S, Rotella F, Marazziti D (2011) Inflammatory and neurodegenerative pathways in depression: a new avenue for antidepressant development? Curr Med Chem 18(2):245–255
Maes M, Smith R, Scharpe S (1995) The monocyte-T-lymphocyte hypothesis of major depression. Psychoneuroendocrinology 20(2):111–116
Maes M, Kubera M, Obuchowiczwa E, Goehler L, Brzeszcz J (2011) Depression’s multiple comorbidities explained by (neuro)inflammatory and oxidative & nitrosative stress pathways. Neuroendocrinol Lett 32(1):7–24
Musselman DL, Miller AH, Porter MR, Manatunga A, Gao F, Penna S, Pearce BD, Landry J, Glover S, McDaniel JS, Nemeroff CB (2011) Higher than normal plasma interleukin-6 concentrations in cancer patients with depression: preliminary findings. Am J Psychiatry 158(8):1252–1257
Lampert R, Bremner JD, Su S, Miller A, Lee F, Cheema F, Goldberg J, Vaccarino V (2008) Decreased heart rate variability is associated with higher levels of inflammation in middle-aged men. Am Heart J 156(4):759.e1–759.e7
Vanuytsel T, Vermeire S, Cleynen I (2013) The role of Haptoglobin and its related protein, zonulin, in inflammatory bowel disease. Tissue Barriers 1(5), e27321
Alayash AI (2011) Haptoglobin: old protein with new functions. Clin Chim Acta 412(7–8):493–498
Quaye IK (2008) Haptoglobin, inflammation and disease. Trans R Soc Trop Med Hyg 102(8):735–742
Rose-John S (2012) IL-6 trans-signaling via the soluble IL-6 receptor: importance for the pro-inflammatory activities of IL-6. Int J Biol Sci 8:1237–1247
Maes M, Meltzer HY, Bosmans E, Bergmans R, Vandoolaeghe E, Ranjan R, Desnyder R (1995) Increased plasma concentrations of interleukin-6, soluble interleukin-6, soluble interleukin-2 and transferrin receptor in major depression. J Affect Disord 34(4):301–309
Maes M, Anderson G, Kubera M, Berk M (2014) Targeting classical IL-6 signalling or IL-6 trans-signalling in depression? Expert Opin Ther Targets 18(5):495–512
Loscalzo J, Kohane I, Barabasi AL (2007) Human disease classification in the postgenomic era: a complex systems approach to human pathobiology. Mol Syst Biol 3:124
López-Muñoz F, Alamo C (2009) Monoaminergic neurotransmission: the history of the discovery of antidepressants from 1950s until today. Curr Pharm Des 15:1563–1586
Moncrieff J, Wessely S, Hardy R (2004) Active placebos versus antidepressants for depression. Cochrane Database Syst Rev 2004, CD003012
Turner EH, Loftis JM, Blackwell AD (2006) Serotonin a la carte: supplementation with the serotonin precursor 5-hydroxytryptophan. Pharmacol Ther 109(3):325–338
Słuzewska A, Rybakowski JK, Laciak M, Mackiewicz A, Sobieska M, Wiktorowicz K (1995) Interleukin-6 serum levels in depressed patients before and after treatment with fluoxetine. Ann N Y Acad Sci 762:474–476
Xia Z, DePierre JW, Nässberger L (1996) Tricyclic antidepressants inhibit IL-6, IL-1 beta and TNF-alpha release in human blood monocytes and IL-2 and interferon-gamma in T cells. Immunopharmacology 34(1):27–37
Maes M, Song C, Lin AH, Bonaccorso S, Kenis G, De Jongh R, Bosmans E, Scharpé S (1999) Negative immunoregulatory effects of antidepressants: inhibition of interferon-gamma and stimulation of interleukin-10 secretion. Neuropsychopharmacology 20(4):370–379
Kenis G, Maes M (2002) Effects of antidepressants on the production of cytokines. Int J Neuropsychopharmacol 5(4):401–412
Hannestad J, DellaGioia N, Bloch M (2011) The effect of antidepressant medication treatment on serum levels of inflammatory cytokines: a meta-analysis. Neuropsychopharmacology 36(12):2452–2459
Munzer A, Sack U, Mergl R, Schönherr J, Petersein C, Bartsch S, Kirkby KC, Bauer K, Himmerich H (2013) Impact of antidepressants on cytokine production of depressed patients in vitro. Toxins (Basel) 5(11):2227–2240
Maes M, Berk M, Goehler L, Song C, Anderson G, Gałecki P (2012) Leonard B (2012) Depression and sickness behavior are Janus-faced responses to shared inflammatory pathways. BMC Med 10:66
Maes M, Mihaylova I, Ruyter MD, Kubera M, Bosmans E (2007) The immune effects of TRYCATs (tryptophan catabolites along the IDO pathway): relevance for depression—and other conditions characterized by tryptophan depletion induced by inflammation. Neuroendocrinol Lett 28(6):826–831
Maes M, Leonard BE, Myint AM, Kubera M, Verkerk R (2011) The new ‘5-HT’ hypothesis of depression: cell-mediated immune activation induces indoleamine 2,3-dioxygenase, which leads to lower plasma tryptophan and an increased synthesis of detrimental tryptophan catabolites (TRYCATs), both of which contribute to the onset of depression. Prog Neuropsychopharmacol Biol Psychiatry 35(3):702–721
Hernansanz-Agustín P, Izquierdo-Álvarez A, García-Ortiz A, Ibiza S, Serrador JM, Martínez-Ruiz A (2013) Nitrosothiols in the immune system: signaling and protection. Antioxid Redox Signal 18(3):288–308
Moylan S, Berk M, Dean OM, Samuni Y, Williams LJ, O’Neil A, Hayley AC, Pasco JA, Anderson G, Jacka FN, Maes M (2014) Oxidative & nitrosative stress in depression: why so much stress? Neurosci Biobehav Rev 45:46–62
García-Bueno B, Madrigal JL, Pérez-Nievas BG, Leza JC (2008) Stress mediators regulate brain prostaglandin synthesis and peroxisome proliferator-activated receptor-gamma activation after stress in rats. Endocrinology 149:1969–1978
García-Bueno B, Caso JR, Leza JC (2008) Stress as a neuroinflammatory condition in brain: damaging and protective mechanisms. Neurosci Biobehav Rev 32:1136–1151
García-Bueno B, Caso JR, Pérez-Nievas BG, Lorenzo P, Leza JC (2007) Effects of peroxisome proliferator-activated receptor gamma agonists on brain glucose and glutamate transporters after stress in rats. Neuropsychopharmacology 32:1251–1260
Maes M (2012) Targeting cyclooxygenase-2 in depression is not a viable therapeutic approach and may even aggravate the pathophysiology underpinning depression. Metab Brain Dis 27(4):405–413
Galecki P, Galecka E, Maes M, Chamielec M, Orzechowska A, Bobin’ska K, Lewin’ski A, Szemraj J (2012) The expression of genes encoding for COX-2, MPO, iNOS, and sPLA2-IIA in patients with recurrent depressive disorder. J Affect Disord 138(3):360–366
Sepanjnia K, Modabbernia A, Ashrafi M, Modabbernia MJ, Akhondzadeh S (2012) Pioglitazone adjunctive therapy for moderate-to-severe major depressive disorder: randomized double-blind placebo-controlled trial. Neuropsychopharmacology 37:2093–2100
O’Neil A, Sanna L, Redlich C, Sanderson K, Jacka F, Williams LJ, Pasco JA (2012) Berk M (2012) The impact of statins on psychological wellbeing: a systematic review and meta-analysis. BMC Med 10:154
Pasco JA, Jacka FN, Williams LJ, Henry MJ, Nicholson GC, Kotowicz MA, Berk M (2010) Clinical implications of the cytokine hypothesis of depression: the association between use of statins and aspirin and the risk of major depression. Psychother Psychosom 79(5):323–325
Stafford L, Berk M (2011) The use of statins after a cardiac intervention is associated with reduced risk of subsequent depression: proof of concept for the inflammatory and oxidative hypotheses of depression? J Clin Psychiatry 72(9):1229–1235
Ghanizadeh A, Hedayati A (2013) Augmentation of fluoxetine with lovastatin for treating major depressive disorder, a randomized double-blind placebo controlled-clinical trial. Depress Anxiety 30(11):1084–1088
Kang J-H, Kao L-T, Lin H-C, Tsai M-C, Chung S-D (2014) Statin Use Increases the Risk of Depressive Disorder in Stroke Patients: A Population-Based Study. J Neurol Sci 2014; Available online 18 November 2014
Tuccori M, Montagnani S, Mantarro S, Capogrosso-Sansone A, Ruggiero E, Saporiti A, Antonioli L, Fornai M, Blandizzi C (2014) Neuropsychiatric adverse events associated with statins: epidemiology, pathophysiology, prevention and management. CNS Drugs 28(3):249–272
Fernandes GH, Zanoteli E, Shinjo SK (2014) Statin-associated necrotizing autoimmune myopathy. Mod Rheumatol 24(5):862–864
Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF, Haroon E, Miller AH (2013) A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry 70(1):31–41
Cimaz R (2008) Lehman T (2008) Pediatrics in systemic autoimmune diseases. In: Asherson RA (ed) Handbook of Systemic Autoimmune Diseases, volume 6. Elsevier, Amsterdam
Saraceno R, Faleri S, Ruzzetti M, Centonze D, Chimenti S (2012) Prevalence and management of panic attacks during infliximab infusion in psoriatic patients. Dermatology 225:236–241
Eshuis EJ, Magnin KM, Stokkers PC, Bemelman WA, Bartelsman J (2010) Suicide attempt in ulcerative colitis patient after 4 months of infliximab therapy—a case report. J Crohn’s Colitis 4(5):591–593
Elisa B, Beny L (2010) Induction of manic switch by the tumour necrosis factor-alpha antagonist infliximab. Psychiatry Clin Neurosci 64(4):442–443
Charles PJ, Smeenk RJ, De Jong J, Feldmann M, Maini RN (2000) Assessment of antibodies to double-stranded DNA induced in rheumatoid arthritis patients following treatment with infliximab, a monoclonal antibody to tumor necrosis factor alpha: findings in open-label and randomized placebo-controlled trials. Arthritis Rheum 43(11):2383–2390
Dodd S, Maes M, Anderson G, Dean OM, Moylan S, Berk M (2013) Putative neuroprotective agents in neuropsychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry 42:135–145
Lai J, Moxey A, Nowak G, Vashum K, Bailey K, McEvoy M (2012) The efficacy of zinc supplementation in depression: systematic review of randomised controlled trials. J Affect Disord 136(1–2):e31–e39
Magalhães PV, Dean OM, Bush AI, Copolov DL, Malhi GS, Kohlmann K, Jeavons S, Schapkaitz I, Anderson-Hunt M, Berk M (2011) N-acetylcysteine for major depressive episodes in bipolar disorder. Rev Bras Psiquiatr 33(4):374–378
Lopresti AL, Maes M, Maker GL, Hood SD, Drummond PD (2014) Curcumin for the treatment of major depression: a randomised, double-blind, placebo controlled study. J Affect Disord 167:368–375
Song C, Zhang XY, Manku M (2009) Increased phospholipase A2 activity and inflammatory response but decreased nerve growth factor expression in the olfactory bulbectomized rat model of depression: effects of chronic ethyl-eicosapentaenoate treatment. J Neurosci 29(1):14–22
Leonard B, Maes M (2012) Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosci Biobehav Rev 36(2):764–785
Schiebinger L, Schraudner M (2011) Interdisciplinary approaches to achieving gendered innovations in science, medicine, and engineering. Interdisc Sci Rev 36:154–167
Vodovotz Y, Csete M, Bartels J, Chang S, An G (2008) Translational systems biology of inflammation. PLoS Comput Biol 4(4), e1000014
Aderem A, Smith KD (2004) A systems approach to dissecting immunity and inflammation. Semin Immunol 16(1):55–67
Cesario A, Auffray C, Agusti A, Apolone G, Balling R, Barbanti P, Bellia A, Boccia S, Bousquet J, Cardaci V, Cazzola M, Dall’Armi V, Daraselia N, Ros LD, Bufalo AD, Ducci G, Ferri L, Fini M, Fossati C, Gensini G, Granone PM, Kinross J, Lauro D, Cascio GL, Lococo F, Lococo A, Maier D, Marcus F, Margaritora S, Marra C, Minati G, Neri M, Pasqua F, Pison C, Pristipino C, Roca J, Rosano G, Rossini PM, Russo P, Salinaro G, Shenhar S, Soreq H, Sterk PJ, Stocchi F, Torti M, Volterrani M, Wouters EF, Frustaci A, Bonassi S (2014) A systems medicine clinical platform for understanding and managing non-communicable diseases. Curr Pharm Des 20(38):5945–5956
Antony PM, Balling R, Vlassis N (2012) From systems biology to systems biomedicine. Curr Opin Biotechnol 23(4):604–608
Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, Amin N, Schwikowski B, Ideker T (2003) Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res 13:2498–2504
Chindelevitch L, Ziemek D, Enayetallah A, Randhawa R, Sidders B, Brockel C, Huang ES (2012) Causal reasoning on biological networks: interpreting transcriptional changes. Bioinformatics 28(8):1114–1121
Feiglin A, Hacohen A, Sarusi A, Fisher J, Unger R, Ofran Y (2012) Static network structure can be used to model the phenotypic effects of perturbations in regulatory networks. Bioinformatics 28(21):2811–2818
Acknowledgments
MB is supported by a NHMRC Senior Principal Research Fellowship (GNT1059660).
Conflict of Interest
MB has received Grant/Research Support from the National Institute of Health (USA), Simons Foundation, CRC for Mental Health, Stanley Medical Research Institute, Medical Benefits Fund, National Health and Medical Research Council (NHMRC of Australia), Beyond Blue, Geelong Medical Research Foundation, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Organon, Novartis, Mayne Pharma, Servier, and Astra Zeneca. He has been a paid consultant for Astra Zeneca, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Janssen Cilag, Lundbeck, and Pfizer and a paid speaker for Astra Zeneca, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Janssen Cilag, Lundbeck, Organon, Pfizer, Sanofi Synthelabo, Solvay, and Wyeth.
Other authors do not report any conflict of interest.
Contributions
All authors contributed equally to the paper.
Funding
There was no specific funding for this specific study.
We confirm that we have read the journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maes, M., Nowak, G., Caso, J.R. et al. Toward Omics-Based, Systems Biomedicine, and Path and Drug Discovery Methodologies for Depression-Inflammation Research. Mol Neurobiol 53, 2927–2935 (2016). https://doi.org/10.1007/s12035-015-9183-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-015-9183-5