Abstract
Purpose of Review
Lifestyle interventions (such as diet and physical activity) successfully limit excessive gestational weight gain and can reduce some adverse maternal events; however, benefit is variable and cost-effectiveness remains unclear. We aimed to review published cost-effectiveness analyses of lifestyle interventions compared with usual care on clinically relevant outcome measures. Five international and six grey-literature databases were searched from 2007 to 2018. Articles were assessed for quality of reporting. Data were extracted from healthcare and societal perspectives. Costs were adapted to the common currencies of Australia and the United Kingdom by adjusting for resource utilization, healthcare purchase price and changes in costs over time. Included studies were economic analyses of lifestyle interventions aiming to limit weight-gain during pregnancy and/or reduce risk of gestational diabetes, for women with a BMI of 25 or greater in pre- or early-pregnancy.
Recent Findings
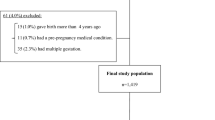
Of the 538 articles identified, six were retained for review: one modelling study and five studies in which an economic analysis was performed alongside a randomized-controlled trial. Outcome measures included infant birth-weight, fasting glucose, insulin resistance, gestational weight-gain, infant respiratory distress syndrome, perceived health, cost per case of adverse outcome avoided and quality-adjusted life years (QALYs). Interventions were cost-effective in only one study.
Summary
Although many studies have investigated the efficacy of lifestyle interventions in pregnancy, few have included cost-effectiveness analyses. Where cost-effectiveness studies were undertaken, results were inconsistent. Secondary meta-analysis, taxonomy and framework research is now required to determine the effective components of lifestyle interventions and to guide future cost-effectiveness analyses.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Dinsdale S, Branch K, Cook L, Shucksmith J. “As soon as you’ve had the baby that’s it...” a qualitative study of 24 postnatal women on their experience of maternal obesity care pathways. BMC Public Health. 2016;16:1–13. https://doi.org/10.1186/s12889-016-3289-1.
• Goldstein RF, Abell SK, Ranasinha S, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA - J Am Med Assoc. 2017;317:2207–25. https://doi.org/10.1001/jama.2017.3635 Findings from this study establish the association between gestational weight gain and maternal and infant outcomes.
World Health Organization. (2018) Obesity. In: Heal. Top. http://www.who.int/topics/obesity/en/. Accessed 20 Feb 2018.
Institute of Medicine and National Research Council Committee to Reexamine IOM Pregnancy Weight Guidelines (2009) Re-examinng IOM Pregnancy Weight Guidelines. In: Rasmussen, K.M. Yaktine A, L. (eds) Weight gain during pregnancy: reexamining the guidelines. National Academies Press, Washington, DC.
Gaillard R. Maternal obesity during pregnancy and cardiovascular development and disease in the offspring. Eur J Epidemiol. 2015;30:1141–52. https://doi.org/10.1007/s10654-015-0085-7.
Cheney K, Farber R, Barratt AL, McGeechan K, de Vries B, Ogle R, et al. Population attributable fractions of perinatal outcomes for nulliparous women associated with overweight and obesity, 1990-2014. Med J Aust. 2018;208:119–25. https://doi.org/10.5694/mja17.00344.
Agha M, Agha RA, Sandell J (2014) Interventions to reduce and prevent obesity in pre-conceptual and pregnant women: a systematic review and meta-analysis. PLoS One 9:. https://doi.org/10.1371/journal.pone.0095132.
Rogozińska E, Marlin N, Jackson L, et al (2017) Effects of antenatal diet and physical activity on maternal and fetal outcomes: individual patient data meta-analysis and health economic evaluation. Health Technol Assess (Rockv) 21:. https://doi.org/10.3310/hta21410.
Farpour-Lambert NJ, Ells LJ, Martinez de Tejada B, Scott C (2018) Obesity and weight gain in pregnancy and postpartum: an evidence review of lifestyle interventions to inform maternal and child health policies. Front Endocrinol (Lausanne) 9:. https://doi.org/10.3389/fendo.2018.00546.
Walker R, Bennett C, Blumfield M, et al. Attenuating pregnancy weight gain—what works and why: a systematic review and meta-analysis. Nutrients. 2018;10:4–6. https://doi.org/10.3390/nu10070944.
•• The International Weight Management in Pregnancy Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta-analysis of individual participant data from randomised trials. BMJ. 2017;358:j3119. https://doi.org/10.1136/bmj.j3119 This study quantifies the effect of lifestyle interventions on maternal and infant outcomes.
Hill B, Skouteris H, Fuller-Tyszkiewicz M. Interventions designed to limit gestational weight gain: a systematic review of theory and meta-analysis of intervention components. Obes Rev. 2013;14:435–50. https://doi.org/10.1111/obr.12022.
Neumann PJ, Farquhar M, Wilkinson CL, Lowry M, Gold M. Lack of cost-effectiveness analyses to address healthy people 2020 priority areas. Am J Public Health. 2016;106:2205–7. https://doi.org/10.2105/AJPH.2016.303361.
Dodd JM, Turnbull D, McPhee AJ, et al. Antenatal lifestyle advice for women who are overweight or obese: LIMIT randomised trial. Obstet Gynecol Surv. 2015;69:311–3. https://doi.org/10.1097/01.ogx.0000451478.28533.cf.
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12:131–41. https://doi.org/10.1111/j.1467-789X.2009.00712.x.
Whiteman VE, Salemi JL, Mejia De Grubb MC, et al. Additive effects of pre-pregnancy body mass index and gestational diabetes on health outcomes and costs. Obesity. 2015;23:2299–308. https://doi.org/10.1002/oby.21222.
Rowlands I, Graves N, de Jersey S, McIntyre H, Callaway L. Obesity in pregnancy: outcomes and economics. Semin Fetal Neonatal Med. 2010;15:94–9. https://doi.org/10.1016/j.siny.2009.09.003.
PDQ- Evidence Database (2018) PDQ-evidence. https://www.pdq-evidence.org/
El-Khayat YM. Resource review. J Med Libr Assoc. 2017;105:431–2. https://doi.org/10.5195/jmla.2017.260.
Thielen FW, Van Mastrigt GAPG, Burgers LT, et al. How to prepare a systematic review of economic evaluations for clinical practice guidelines: database selection and search strategy development (part 2/3). Expert Rev Pharmacoecon Outcomes Res. 2016;16:705–21. https://doi.org/10.1080/14737167.2016.1246962.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339. https://doi.org/10.1136/bmj.b2700.
Veritas Health Innovation (2018) Covidence systematic review software. Available at www.covidence.org
Husereau D, Drummond M, Petrou S, et al. Consolidated health economic evaluation reporting standards (CHEERS)--explanation and elaboration: a report of the ISPOR health economic evaluations publication guidelines task force. Value Health. 2013;16:231–50. https://doi.org/10.1016/j.jval.2013.02.002.
Ademi Z, Tomonaga Y, Van Stiphout J, et al. Adaptation of cost-effectiveness analyses to a single country: the case of bariatric surgery for obesity and overweight. Swiss Med Wkly. 2018;148:1–13. https://doi.org/10.4414/smw.2018.14626.
Organisation for Economic Co-operation and Development (2018) Health spending (indicator). https://data.oecd.org/healthres/health-spending.htm. Accessed 2 Aug 2018.
Organisation for Economic Co-operation and Development (2018) Purchasing power parities (PPP) (indicator).
Australian Institute of Health and Welfare (2018) Health expenditure Australia 2016–17. Canberra.
Office for National Statistics (2018) Reference table 3: Growth rates and indices for public service healthcare inputs, quantity and quality adjusted output and productivity, 1995 to 2015. https://www.ons.gov.uk/economy/economicoutputandproductivity/publicservicesproductivity/datasets/growthratesandindicesforpublicservicehealthcareinputsquantityandqualityadjustedoutputandproductivity. Accessed 2 Aug 2018.
Appleby J, Devlin N, Parkin D. NICE’s cost effectiveness threshold. BMJ. 2007;335:358–9.
Paris V, Belloni A. Value in pharmaceutical pricing. OECD Heal Work Pap. 2013;63:1–74. https://doi.org/10.1787/5k43jc9v6knx-en.
Edney LC, Haji Ali Afzali H, Cheng TC, Karnon J. Estimating the reference incremental cost-effectiveness ratio for the Australian health system. Pharmacoeconomics. 2018;36:239–52. https://doi.org/10.1007/s40273-017-0585-2.
Dodd JM, Ahmed S, Karnon J, Umberger W, Deussen AR, Tran T, et al. The cost-effectiveness of providing antenatal lifestyle advice for women who are overweight or obese: the LIMIT randomised trial. BMC Obes. 2015;2:1–9. https://doi.org/10.1186/s40608-015-0046-4.
Kolu P, Raitanen J, Rissanen P, Luoto R (2013) Cost-effectiveness of lifestyle counselling as primary prevention of gestational diabetes mellitus: findings from a cluster-randomised trial PLoS One 8:. https://doi.org/10.1371/journal.pone.0056392.
Oostdam N, Bosmans J, Woulters MGAJ, et al (2012) Cost-effectiveness of an exercise program during pregnancy to prevent gestational diabetes: results of an economic evaluation alongside a randomised controlled trial BMC Pregnancy Childbirth 12
Poston L, Bell R, Briley AL, et al. Improving pregnancy outcome in obese women: the UK pregnancies better eating and activity randomised controlled trial. Program Grants Appl Res. 2017;5:1–414. https://doi.org/10.3310/pgfar05100.
Broekhuizen K, Simmons D, Devlieger R, van Assche A, Jans G, Galjaard S, et al. Cost-effectiveness of healthy eating and/or physical activity promotion in pregnant women at increased risk of gestational diabetes mellitus: economic evaluation alongside the DALI study, a European multicenter randomized controlled trial. Int J Behav Nutr Phys Act. 2018;15:1–12. https://doi.org/10.1186/s12966-018-0643-y.
Van Reenen M, Janssen B (2015) EQ-5D-5L user guide. Rotterdam.
Sintonen H (2018) The health state desctiptive system (questionnaire. In: 15d-instrument. http://www.15d-instrument.net/15d/the-health-state-descriptive-system/. Accessed 17 Dec 2018.
Gray AM, Clarke PM, Wolstenholme J, Wordsworth S. Applied methods of cost-effectiveness analysis in healthcare. Oxford: Oxford University Press; 2011.
World Health Organization (2016) Report of the commission on ending childhood obesity. Geneva.
Redman LM, Gilmore LA, Breaux J, et al. Effectiveness of SmartMoms, a novel eHealth intervention for Management of Gestational Weight Gain: randomized controlled pilot trial. JMIR Mhealth Uhealth. 2017;5:e133. https://doi.org/10.2196/mhealth.8228.
Lau Y, Klainin-Yobas P, Htun TP, Wong SN, Tan KL, Ho-Lim ST, et al. Electronic-based lifestyle interventions in overweight or obese perinatal women: a systematic review and meta-analysis. Obes Rev. 2017;18:1071–87.
Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:1–12. https://doi.org/10.1136/bmj.g1687.
Harrison CL, Skouteris H, Boyle J, Teede HJ. Preventing obesity across the preconception, pregnancy and postpartum cycle: implementing research into practice. Midwifery. 2017;52:64–70. https://doi.org/10.1016/j.midw.2017.06.003.
Skouteris H, Huang T, Millar L, et al. A systems approach to reducing maternal obesity: the health in preconception, pregnancy and postbirth (HIPPP) collaborative. Aust New Zeal J Obstet Gynaecol. 2015;55:397–400. https://doi.org/10.1111/ajo.12341.
Hill B, McPhie S, Moran LJ, Harrison P, Huang TT, Teede H, et al. Lifestyle intervention to prevent obesity during pregnancy: implications and recommendations for research and implementation. Midwifery. 2017;49:13–8. https://doi.org/10.1016/j.midw.2016.09.017.
Fitria N, van Asselt ADI, Postma MJ. Cost-effectiveness of controlling gestational diabetes mellitus: a systematic review. Eur J Health Econ. 2018;20:407–17. https://doi.org/10.1007/s10198-018-1006-y.
Funding
CB acknowledges funding support from the Australian Prevention Partnership Centre. BdC is a recipient of the National Heart Foundation (NHF future leader fellowship 100864). HT is a recipient of NHMRC Practitioner fellowship. BH is funded by an NHMRC Early Career Fellowship (GNT1120477).
Author information
Authors and Affiliations
Contributions
CB developed the search strategy, led the data collection and analysis and wrote the initial draft of the manuscript. ZA contributed in the design and scope of search strategy, advised on all aspects of the methodology and contributed expertise to the revision and editing of the manuscript. HS contributed to the conceptualization of the study, the design and scope of the search strategy and revised and edited the manuscript. BH contributed to reviewing data collection and revised and edited the manuscript. HT and BdC contributed to conceptualization of the study and revised and edited the manuscript. DL, RW and ST revised and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Cate Bailey, Helen Skouteris, Helena Teede, Briony Hill, Barbora De Courten, Ruth Walker, Danny Liew, Shakila Thangaratinam and Zanfina Ademi each declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Diabetes and Pregnancy
Electronic supplementary material
ESM 1
(DOCX 181 kb)
Rights and permissions
About this article
Cite this article
Bailey, C., Skouteris, H., Teede, H. et al. Are Lifestyle Interventions to Reduce Excessive Gestational Weight Gain Cost Effective? A Systematic Review. Curr Diab Rep 20, 6 (2020). https://doi.org/10.1007/s11892-020-1288-1
Published:
DOI: https://doi.org/10.1007/s11892-020-1288-1