Abstract
Purpose
The validity of the SF-6D, a preference-based measure of health-related quality of life, is not well explored in the context of spinal cord injury (SCI). The aim of this analysis was to assess appropriate measurement properties of the SF-6D in a sample of individuals living with SCI.
Methods
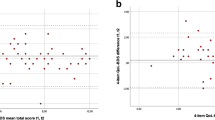
Longitudinal data from the Rick Hansen Spinal Cord Injury Registry were used. Responses to the 36-item short-form health survey were transformed into SF-6D utility scores. We investigated practicality, floor and ceiling effects, and responsiveness to change. Responsiveness to change was explored using three different anchors that reflected changes in self-reported health, functional independence, and life satisfaction. Discriminative validity was assessed by ten a priori defined hypotheses, with a distinction made between ‘strong’ and ‘weak’ hypotheses.
Results
Three hundred and fifty-eight individuals with SCI were included in this analysis. Practicality was deemed acceptable based on a completion rate of 94 %. The SF-6D showed low responsiveness to detect important health changes over time, and differences in responsiveness were found between individuals with paraplegia and tetraplegia. All five strong hypotheses and three weak hypotheses were confirmed.
Conclusion
The SF-6D demonstrated good practicality and discriminative validity in this sample. The failure to detect self-reported and clinically important health changes requires further consideration. Comparative performance of the SF-6D (i.e., how the SF-6D performs against other preference-based measures) is unknown in the SCI context and requires further research.


Similar content being viewed by others
References
Strauss, D. J., Devivo, M. J., Paculdo, D. R., & Shavelle, R. M. (2006). Trends in life expectancy after spinal cord injury. Archives of Physical Medicine and Rehabilitation, 87(8), 1079–1085.
Torrance, G. W. (1986). Measurement of health state utilities for economic appraisal. Journal of Health Economics, 5(1), 1–30.
Arnold, D., Girling, A., Stevens, A., & Lilford, R. (2009). Comparison of direct and indirect methods of estimating health state utilities for resource allocation: Review and empirical analysis. British Medical Journal, 339, b2688.
Dolan, P., Olsen, J. A., Menzel, P., & Richardson, J. (2003). An inquiry into the different perspectives that can be used when eliciting preferences in health. Health Economics, 12(7), 545–551.
Brazier, J., Roberts, J., & Deverill, M. (2002). The estimation of a preference-based measure of health from the SF-36. Journal of Health Economics, 21(2), 271–292.
Brazier, J. E., & Roberts, J. (2004). The estimation of a preference-based measure of health from the SF-12. Medical Care, 42(9), 851–859.
Brazier, J. E., Fukuhara, S., Roberts, J., Kharroubi, S., Yamamoto, Y., Ikeda, S., et al. (2009). Estimating a preference-based index from the Japanese SF-36. Journal of Clinical Epidemiology, 62(12), 1323–1331.
Cruz, L. N., Camey, S. A., Hoffmann, J. F., Rowen, D., Brazier, J. E., Fleck, M. P., et al. (2011). Estimating the SF-6D value set for a population-based sample of Brazilians. Value in Health, 14(5 Suppl 1), S108–S114.
Ferreira, L. N., Ferreira, P. L., Pereira, L. N., Brazier, J., & Rowen, D. (2010). A Portuguese value set for the SF-6D. Value in Health, 13(5), 624–630.
Lam, C. L., Brazier, J., & McGhee, S. M. (2008). Valuation of the SF-6D health states is feasible, acceptable, reliable, and valid in a Chinese population. Value in Health, 11(2), 295–303.
Mendez, I., Abellan Perpinan, J. M., Sanchez Martinez, F. I., & Martinez Perez, J. E. (2011). Inverse probability weighted estimation of social tariffs: An illustration using the SF-6D value sets. Journal of Health Economics, 30(6), 1280–1292.
Lee, B. B., King, M. T., Simpson, J. M., Haran, M. J., Stockler, M. R., Marial, O., et al. (2008). Validity, responsiveness, and minimal important difference for the SF-6D health utility scale in a spinal cord injured population. Value in Health, 11(4), 680–688.
Whitehurst, D. G., Noonan, V. K., Dvorak, M. F., & Bryan, S. (2012). A review of preference-based health-related quality of life questionnaires in spinal cord injury research. Spinal Cord, 50(9), 646–654.
Brazier, J., & Deverill, M. (1999). A checklist for judging preference-based measures of health related quality of life: Learning from psychometrics. Health Economics, 8(1), 41–51.
Noonan, V. K., Kwon, B. K., Soril, L., Fehlings, M. G., Hurlbert, R. J., Townson, A., et al. (2012). The Rick Hansen Spinal Cord Injury Registry (RHSCIR): A national patient-registry. Spinal Cord, 50(1), 22–27.
Brazier, J., Rowen, D., & Hanmer, J. (2008). Revised SF-6D scoring programmes: A summary of improvements. PRO Newsletter, 40, 14–15.
Fugl-Meyer, A. R., Bränholm, I.-B., & Fugl-Meyer, K. S. (1991). Happiness and domain specific life satisfaction in adult northern Swedes. Clinical Rehabilitation, 5, 25–33.
Keith, R. A., Granger, C. V., Hamilton, B. B., & Sherwin, F. S. (1987). The functional independence measure: A new tool for rehabilitation. Advances in Clinical Rehabilitation, 1, 6–18.
Anderson, K., Aito, S., Atkins, M., Biering-Sorensen, F., Charlifue, S., Curt, A., et al. (2008). Functional recovery measures for spinal cord injury: An evidence-based review for clinical practice and research. The Journal of Spinal Cord Medicine, 31(2), 133–144.
Whiteneck, G. G., Harrison-Felix, C. L., Mellick, D. C., Brooks, C. A., Charlifue, S. B., & Gerhart, K. A. (2004). Quantifying environmental factors: A measure of physical, attitudinal, service, productivity, and policy barriers. Archives of Physical Medicine and Rehabilitation, 85(8), 1324–1335.
Terwee, C. B., Bot, S. D., de Boer, M. R., van der Windt, D. A., Knol, D. L., Dekker, J., et al. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology, 60(1), 34–42.
Fayers, P. M., & Machin, D. (2000). Quality of life: Assessment, analysis and interpretation. Chichester, West Sussex: Wiley.
Lam, T., Noonan, V. K., & Eng, J. J. (2008). A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord, 46(4), 246–254.
Post, M. (2010). Measuring the subjective appraisal of participation with life satisfaction measures: Bridging the gap between participation and quality of life measurement. Topics in Spinal Cord Injury Rehabilitation, 15(4), 1–15.
Post, M. W., van Leeuwen, C. M., van Koppenhagen, C. F., & de Groot, S. (2012). Validity of the life satisfaction questions, the life satisfaction questionnaire, and the satisfaction with life scale in persons with spinal cord injury. Archives of Physical Medicine and Rehabilitation, 93(10), 1832–1837.
Cohen, J. (1988). Statistical power analysis for the behavioural sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum.
Gurcay, E., Bal, A., Eksioglu, E., & Cakci, A. (2010). Quality of life in patients with spinal cord injury. International Journal of Rehabilitation Research, 33(4), 356–358.
Haran, M. J., Lee, B. B., King, M. T., Marial, O., & Stockler, M. R. (2005). Health status rated with the medical outcomes study 36-item short-form health survey after spinal cord injury. Archives of Physical Medicine and Rehabilitation, 86(12), 2290–2295.
Vogel, L. C., Krajci, K. A., & Anderson, C. J. (2002). Adults with pediatric-onset spinal cord injuries: Part 3: Impact of medical complications. Journal of Spinal Cord Medicine, 25(4), 297–305.
Westgren, N., & Levi, R. (1998). Quality of life and traumatic spinal cord injury. Archives of Physical Medicine and Rehabilitation, 79(11), 1433–1439.
IBM Corp. (2010). IBM SPSS statistics for Windows, Version 19.0. Armonk, NY: IBM Corp.
StataCorp. (2011). Stata statistical software: Release 12. College Station, TX: StataCorp LP.
Meyers, A. R., Andresen, E. M., & Hagglund, K. J. (2000). A model of outcomes research: Spinal cord injury. Archives of Physical Medicine and Rehabilitation, 81(12 Suppl 2), S81–S90.
Liang, M. H. (2000). Longitudinal construct validity: Establishment of clinical meaning in patient evaluative instruments. Medical Care, 38(9 Suppl), II84–II90.
Sprangers, M. A., & Schwartz, C. E. (1999). Integrating response shift into health-related quality of life research: A theoretical model. Social Science and Medicine, 48(11), 1507–1515.
Weitzenkamp, D., Gerhart, K., Charlifue, S., Whiteneck, G., Glass, C., & Kennedy, P. (2000). Ranking the criteria for assessing quality of life after disability: Evidence for priority shifting among long-term spinal cord injury survivors. British Journal of Health Psychology, 5(1), 57–69.
Whitehurst, D. G., & Mittmann, N. (2013). The value of health economics research in spinal cord injury. Spinal Cord, 51(8), 586–587.
Krahn, G. L., Fujiura, G., Drum, C. E., Cardinal, B. J., & Nosek, M. A. (2009). The dilemma of measuring perceived health status in the context of disability. Disability and Health Journal, 2(2), 49–56.
Putzke, J. D., Richards, J. S., Hicken, B. L., & DeVivo, M. J. (2002). Predictors of life satisfaction: A spinal cord injury cohort study. Archives of Physical Medicine and Rehabilitation, 83(4), 555–561.
Post, M., & Noreau, L. (2005). Quality of life after spinal cord injury. Journal of Neurologic Physical Therapy, 29(3), 139–146.
Johnson, R. L., Gerhart, K. A., McCray, J., Menconi, J. C., & Whiteneck, G. G. (1998). Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord, 36(1), 45–50.
Leduc, B. E., & Lepage, Y. (2002). Health-related quality of life after spinal cord injury. Disability and Rehabilitation, 24(4), 196–202.
McColl, M. A., Arnold, R., Charlifue, S., Glass, C., Savic, G., & Frankel, H. (2003). Aging, spinal cord injury, and quality of life: structural relationships. Archives of Physical Medicine and Rehabilitation, 84(8), 1137–1144.
Stensman, R. (1994). Adjustment to traumatic spinal cord injury. A longitudinal study of self-reported quality of life. Paraplegia, 32(6), 416–422.
Kreuter, M., Siosteen, A., Erkholm, B., Bystrom, U., & Brown, D. J. (2005). Health and quality of life of persons with spinal cord lesion in Australia and Sweden. Spinal Cord, 43(2), 123–129.
Holicky, R., & Charlifue, S. (1999). Ageing with spinal cord injury: The impact of spousal support. Disability and Rehabilitation, 21(5–6), 250–257.
Putzke, J. D., Elliott, T. R., & Richards, J. S. (2001). Marital status and adjustment 1 year post-spinal-cord-injury. Journal of Clinical Psychology in Medical Settings, 8(2), 101–107.
Acknowledgments
This work has been conducted without financial support, and the authors declare no conflict of interest. We would like to thank the Rick Hansen Institute for the provision of the data and Dr. Penny Brasher for her contribution to the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Engel, L., Bryan, S., Evers, S.M.A.A. et al. Exploring psychometric properties of the SF-6D, a preference-based health-related quality of life measure, in the context of spinal cord injury. Qual Life Res 23, 2383–2393 (2014). https://doi.org/10.1007/s11136-014-0677-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-014-0677-9