Abstract
Decision-making deficits are strong predictors of poor clinical outcomes in addiction treatment. However, research on interventions that address decision-making deficits among people with addiction is scarce and has not been analyzed. We aimed to systematically review evidence on neuropsychological interventions for decision-making deficits in addiction to identify promising therapies. Eligibility criteria were (1) participants with a diagnosis of substance use or behavioral addictive disorders, (2) interventions consisting of (neuro) psychological treatments that address decision-making, (3) comparators comprising control (sham) interventions, treatment as usual or no-treatment, (4) outcomes including a decision-making task, and (5) studies including RCTs and non-randomized trials. Search terms included addiction (or alcohol/drug/substance use/gambling) AND treatment (or specific interventions) AND decision-making (or specific tasks). The search yielded 728 hits, and two independent assessors agreed on the final selection of 12 articles. Interventions included Contingency Management (3 studies), Working Memory Training (2 studies) Goal Management Training (2 studies), Cognitive Behavioral Therapy (2 studies), Reality Therapy, Motivational Interview and Monetary Management. The main outcome measures were tasks of delay discounting, risk-taking and reward-based decision-making. Results showed that Goal Management Training improves reward-based decision-making, while Contingency Management combined with Cognitive Behavioral Therapy has beneficial effects on delay discounting. The evidence on Working Memory Training and Cognitive Behavioral Therapy as stand-alone treatments was mixed. Motivational Interview and Monetary Management had no significant effects on decision-making. Bias control across studies was moderate. We conclude that Goal Management Training and Contingency Management combined with Cognitive Behavioral Therapy have potential to modify decision-making in people with addiction. RCTs are needed to establish the efficacy of these interventions.
Similar content being viewed by others
Introduction
Addictive disorders involve excessive, often uncontrolled drug use or gambling despite clear negative consequences for health, productivity and social relationships (American Psychiatric Association 2013). This description suggests an underlying dysfunction of decision-making skills. Early insights about this notion ignited a large body of neuropsychology research that observed decision-making deficits in people with addiction (Bechara and Damasio 2002; Bechara et al. 2001; Bechara et al. 2002; Goudriaan et al. 2005; Grant et al. 2000; see Verdejo-García et al. 2018 for a recent review). In a nutshell, they observed decision-making patterns that are heavily influenced by immediate rewards (via positive or negative reinforcement), and less influenced by the future value of available options (Noël et al. 2013). The leverage of immediate rewards relates to sensitization of the “reward system” (the dopaminergic mesolimbic system), which prioritizes stimuli that yield fast and intense reward outcomes (Robinson and Berridge 2008). Reduced influence of future outcomes relates to impulsivity (acting without planning), or weakened cognitive or affective representations of the value of future states (Bechara 2005). The latter deficits are linked to abnormalities in the “cognitive control system” (the dorsolateral prefrontal cortex, anterior cingulate and their connections with the striatum) or the “emotional system” (the ventromedial prefrontal cortex, amygdala and insula: Noël et al. 2013; Redish et al. 2008; Verdejo-García and Bechara 2009).
The significance of decision-making deficits in the context of addiction is clearly illustrated by meaningful associations between these deficits and higher risk of transitioning between recreational and harmful use (Stewart et al. 2017; Stewart et al. 2013), and drug relapse after treatment (Stevens et al. 2015; Verdejo-Garcia et al. 2014). Moreover, retuning of reward values and re-engagement with future goals is frequently reported in the context of natural recovery from addiction (Heyman 2009). Given the relevance of decision-making for addiction liability and recovery, psychological interventions targeting decision-making skills are well poised to make a difference in the context of addiction treatment. Unfortunately, very few therapeutic approaches have specifically focused on decision-making mechanisms. The available options can be grouped in two main families (1) neuropsychological interventions, including strategy-based cognitive rehabilitation and exercise-based cognitive training (e.g., rehabilitation of executive functions, working memory training), and (2) psychological interventions that address reward learning and cognitive control (e.g., contingency management, cognitive behavioral therapy). The first group uses neuropsychology principles (brain-behavior relations) to inform therapeutic strategies and exercises aimed to modify cognitive, including decision-making, skills. The second group uses general principles of cognitive-behavior change, such as operant learning and cognitive restructuring, to modify cognitive beliefs and behavioral patterns. As many of these beliefs and patterns are directly linked to decision-making, these strategies can indirectly address decision-making mechanisms. In the following lines, we briefly describe the specific approaches that directly or indirectly are aimed at neurocognitive systems of decision-making.
In the context of neuropsychological interventions, Goal Management Training is a comprehensive, interactive program aimed to retrain executive functions (Levine et al. 2007). Relevant to decision-making, Goal Management Training places specific emphasis on goal-based strategies that can override automatic responses including reward-driven behaviors and habits (Levine et al. 2011). It also includes a specific module on decision-making, which focuses on training a mindful, goal-focused approach to complex decisions. With regard to cognitive training, computerized Working Memory Training has been proposed to reduce impulsive decision-making (Bickel et al. 2014). The rationale here is that working memory exercises can strengthen the cognitive control system, and hence boost cognitive representations of future goals (Wesley and Bickel 2014). In the context of psychological interventions, Contingency Management is a relatively specific approach to modify the “reward system” of decision-making (Shoptaw 2014). Contingency Management typically consists of exchanging evidence of abstinence (e.g., negative drug tests) for valuable rewards (e.g., monetary vouchers). In this way, the intervention replaces drug rewards with another powerful and immediate incentive, contributing to progressive normalization of the “brain reward system”, and modification of decision-making priorities (Stanger et al. 2013). More generally, Cognitive Behavioral Therapy tackles some of the thinking bases of dysfunctional decision-making (e.g., the belief that craving reflects the “need” to take drugs or gamble) and trains specific goal-oriented strategies such as relapse prevention. Third-generation therapies, such as Mindfulness, Motivational Interview or Reality Therapy, focus on reconciling goals with motivations and emotions. By strengthening these links, they can potentially increase cognitive and emotional representations of goal states, and indirectly improve cognitive control (Feldstein Ewing et al. 2011).
A first step towards assessing the usefulness of the interventions described above in the context of addiction treatment is to evaluate their impact on cognitive measures of decision-making. Based on neuropsychological models of decision-making, we considered outcomes related to four cognitive mechanisms (1) reflection-impulsivity, (2) delay discounting, (3) decision-making under risk, and (4) decision-making under ambiguity (Schiebener and Brand 2015; Verdejo-García et al. 2018). Reflection impulsivity refers to the amount of information that is collected before making a decision, either in open situations or within a “risk-reward trade-off scenario” where gathering more information is linked to less reward (Clark et al. 2006). Delay discounting relates to choices between lower immediate rewards and larger more delayed rewards (e.g., between $5 now and $50 in 3 months: Bickel and Marsch 2001). Decision-making under risk, or risk-taking, consists on choosing between options that contain explicit information about their outcomes. Conversely, decision-making under uncertainty involves choices between options with unknown or hardly accessible outcomes (Brand et al. 2006). Most of these cognitive paradigms involve conflict between immediate reward and long-term goals. Therefore, they mimic the decision-making deficits observed in people with addictive disorders, although it is often difficult to disambiguate if poor decisions are driven by reward sensitization, “myopia for the future” or both (Bechara 2005). Although more specific measures of the reward and goal systems have been developed (Daw et al. 2011), these measures have not yet permeated intervention studies.
This study aims to systematically review the evidence on neuropsychological and psychological interventions for decision-making deficits in the context of addiction. Specifically, we tested the effect of interventions that directly or indirectly address the neurocognitive mechanisms of decision-making on performance in cognitive measures of decision-making among clinical populations with addictive disorders, including substance use and behavioral addictions. Although recent narrative reviews have provided scientific foundations for the therapeutic potential of neuropsychological interventions in the context of addiction (Rezapour et al. 2016; Verdejo-Garcia 2016), no previous reviews have focused on decision-making interventions or adopted a systematic approach. We sought to provide initial evidence for the usefulness of psychological or neuropsychological interventions that address decision-making skills in the context of addiction, and to distil information about which interventions or aspects of the interventions are more promising to inform further research. Our working hypothesis was that selected interventions would produce significant improvement of decision-making skills, with better results for those interventions that directly target the neurocognitive systems of decision-making, namely, reward, emotion and cognitive control.
Methods
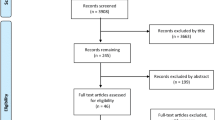
We conducted a systematic review, reported in alignment with the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines (PRISMA; Liberati et al. 2009). The PRISMA checklist is provided in Supplementary Material.
Protocol and Registration
The review protocol has not been specified or published in advance.
Eligibility Criteria
The eligibility criteria were defined as follows (1) participants of both genders aged ≥18 with a diagnosis of substance use or behavioral addictive disorders, (2) interventions consisting of neuro-psychological treatments and psychosocial interventions that address decision-making skills, (3) comparators comprising control or sham interventions (i.e., matched to the active intervention in appearance and exposure but lacking active ingredients) or treatment as usual (e.g., Cognitive Behavioral Therapy, therapeutic community) or no-treatment (i.e., control participants underwent pre-post assessments, but they did not receive any psychological or neuropsychological intervention), (4) outcome measures including at least one cognitive task of decision-making (as defined in the Introduction section), (5) study designs including randomized controlled trials (RCT) and non-randomized trials.
Information Sources
We only considered studies in English, published or ahead of print in peer-reviewed journals, and did not impose limits on year of publication. Studies were identified by searching electronic databases and inspecting reference lists of articles. This search was applied to Scopus (29 August 2017–8 September 2017), Pubmed and PsycINFO (in both cases 29 August 2017–11 September 2017). The last search was conducted on 11 September 2017.
Search
We used the following search terms to search all databases: addiction (or alcohol/drug/substance use/gambling) AND treatment (or intervention or specific exemplars e.g. contingency management, cognitive training) AND decision-making (or specific tasks e.g., Iowa Gambling Task: see details in Supplementary Material, Table S1). We excluded book chapters, letters and editorials, as well as studies including participants with a primary diagnosis of other psychiatric disorders and pharmacological treatments. Although reviews were included in the search to scan reference lists for identification of studies that met inclusion criteria, they were ineligible for inclusion.
Study Selection
The eligibility assessment was conducted independently by two reviewers (AVG and MAC) using an unblinded, standardized, systematic approach employing the software Rayyan (Ouzzani et al. 2016). Disagreements between the two reviewers were resolved via discussion and consensus.
Data Collection Process and Data Items
We developed a data extraction table including the following variables: authors, publication year, country, participants (gender, age), diagnoses, interventions, comparators, duration and intensity of interventions and comparators, design, setting, outcomes, and means and standard deviations (SDs) for outcome measures. When means and SDs were not available, we requested them from the respective study corresponding authors via email. The data were coded as non-reported when two successive emails were unanswered.
Summary Measures
The key summary measure was the effect size of the standardized mean difference between the intervention and the comparator, expressed in Hedge’s g with 95% confidence interval. Hedge’s g was calculated using the formula described by Morris (2008) and detailed by Huntley et al. (2015), which is based on the mean pre-post change in the intervention group minus the mean pre-post change in the comparator group, divided by the pooled pre-intervention standard deviation. We also computed the measure of effect in absolute units, that is, raw difference in mean change scores between the intervention and the comparator with 95% confidence interval, using the formulas defined by the Agency for Healthcare Research and Quality (Fu et al. 2013). Note that absolute effects are not comparable across studies, unlike Hedge's g, and need to be interpreted in terms of the respective means and standard deviations of the measures reported (see Supplementary Material, Table S2).
Risk of Bias
Two independent assessors (MAC and NAU) evaluated the risk of bias across studies using the 13-item scale developed by Thompson et al. (2017) for systematic reviews on intervention studies. We chose Thompson’s scale over other well-validated measures of risk of bias in randomized trials (e.g., Higgins et al. 2011) because its items were more representative of the designs and methodologies of the majority of the selected studies, which were mostly non-randomized trials or secondary analyses of RCTs.
Planned Method of Analysis
We chose not to perform a meta-analysis, given the multiple sources of heterogeneity in terms of study designs, treatment approaches and outcome measures scattered among different cognitive domains of decision-making, as well as the limited (or lack of) outcome data reported in some of the selected studies. Thus, we adopted a narrative approach to discuss the findings of selected studies.
Results
Search Results
Results are displayed in Fig. 1. Our search identified 842 hits and 728 unique articles after removal of duplicates (see details in Supplementary Material, Table S3). One article (Valls-Serrano et al. 2016) was manually added at this stage. After inspection of titles and abstracts we kept 27 articles to read in full. Based on consensus between the two assessors, 12 of 27 were selected for analysis. Reasons for exclusion were lack of neuropsychological or psychological interventions, adequate comparators, or cognitive tasks of decision-making among the outcome measures.
The 12 selected articles included three studies using Contingency Management (Kiluk et al. 2017; Peters et al. 2013; Weidberg et al. 2015), two studies using Working Memory Training (Bickel et al. 2011; Rass et al. 2015), two studies using Goal Management Training (Alfonso et al. 2011; Valls-Serrano et al. 2016), two studies using Cognitive Behavioral Therapy (Carroll et al. 2011; Tavakolian and Abolghasemi 2016), and one study using each of the following interventions, Advisor-Teller Money Management (Black and Rosen 2011), Chess training plus Motivational Interview (Gonçalves et al. 2014), and Reality Therapy (Yao et al. 2017).
Summary of Study Designs
All studies were conducted among clinical populations, 5 in miscellaneous substance users, 2 in opioid users, 2 in cocaine or amphetamine users, and 1 in each of the following: tobacco, marijuana and Internet gaming). We included the Internet gaming study, as this is recognized as a relevant clinical entity by current diagnostic and classification systems (American Psychiatric Association 2013; World Health Organisation 2016). Most studies had small sample sizes (range: 27–116 participants). Only one study was a randomized controlled trial (RCT) specifically designed to test the impact of the active intervention on cognitive decision-making measures (Rass et al. 2015). The remaining studies were secondary analyses of a larger RCT (Black and Rosen 2011; Carroll et al. 2011; Peters et al. 2013; Weidberg et al. 2015), and pilot and proof of concept studies (Alfonso et al. 2011; Bickel et al. 2011; Gonçalves et al. 2014; Kiluk et al. 2017; Tavakolian and Abolghasemi 2016; Valls-Serrano et al. 2016; Yao et al. 2017).
Most studies compared the active intervention with treatment as usual (Alfonso et al. 2011; Carroll et al. 2011; Valls-Serrano et al. 2016), sham training (Bickel et al. 2011; Black and Rosen 2011; Rass et al. 2015) or no-treatment (Tavakolian and Abolghasemi 2016; Yao et al. 2017). In Peters et al. (2013) and Weidberg et al. (2015) Contingency Management was tested in the context of Cognitive Behavioral Therapy (i.e., Contingency Management plus Cognitive Behavioral Therapy versus Cognitive Behavioral Therapy alone). In Kiluk et al. (2017) Contingency Management was tested in the context of Cognitive Remediation Training (i.e., Contingency Management plus Cognitive Remediation Training versus Cognitive Remediation Training alone), and incentives were paired with Cognitive Remediation Training progress. Some studies combined more than one intervention in the active condition. In Bickel et al. (2011) Working Memory Training was motivated with monetary reimbursements, which is a form of Contingency Management. In Gonçalves et al. (2014) Motivational Interviewing was combined with Chess training, an ecological approach to cognitive remediation. Moreover, Goal Management Training and Reality Therapy studies included mindfulness practice. Notwithstanding these treatment schedule complications, we present the findings organized by main active intervention tested.
The outcome measures of decision-making included (1) reflection impulsivity, measured by the Information Sampling Task (Clark et al. 2006), (2) delay discounting, measured with hypothetical tests such as computerized tasks with adaptive procedures to estimate discounting rates (Holt et al. 2012; Johnson et al. 2007) and the Monetary Choice Questionnaire (Kirby et al. 1999) or experiential tasks that provide actual monetary incentives (Reynolds and Schiffbauer 2004), (3) risk-taking, measured with the Balloon Analogue Risk Task (Lejuez et al. 2002), and (4) decision-making under uncertainty, measured by the Iowa Gambling Task (Bechara et al. 2000).
Findings Grouped by Intervention
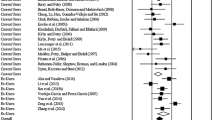
Table 1 provides a summary of the 12 studies selected, including description of design, active and control intervention conditions, sample size and participants, treatment setting, outcome measures, main findings and effect sizes, as well as bias scores.
Goal Management Training
Two studies by the same group have tested Goal Management Training plus treatment as usual (TAU) versus TAU alone among participants with miscellaneous substance use disorders and polysubstance use patterns (Alfonso et al. 2011; Valls-Serrano et al. 2016). Goal Management Training included mindfulness practice, response inhibition training and goal monitoring and decision-making strategies. In Alfonso et al. 2011 TAU consisted of community-based counseling and relapse prevention, whereas in Valls-Serrano et al. 2016 TAU was residential therapeutic community treatment. In Valls-Serrano et al. (2016), but not Alfonso et al. (2011), participants were randomized to treatment conditions, and in both studies the treatment groups were matched on relevant background characteristics (age, years of education, lifetime drug use). Outcomes consisted of tasks of executive functions and decision-making, including reflection impulsivity, namely, Information Sampling Task (Valls-Serrano et al. (2016) and decision-making under uncertainty, namely, Iowa Gambling Task (Alfonso et al. (2011). The two studies showed significant time by treatment interaction effects on key outcomes, that is, participants enrolled in Goal Management Training performed significantly better than those in TAU on the Iowa Gambling Task and the Information Sampling Task after 7 to 8 weeks of training. In Alfonso et al. (2011), the Hedges’s g was 0.85 (95% CI -4.20, 5.90) for the Iowa Gambling Task scores and the absolute measure of effect was 12.69 (95% CI 4.38, 21.00). In Valls-Serrano et al. (2016), the Hedges’s g were 0.69 (95% CI -0.69, 2.07) and − 0.89 (95% CI -1.36, −0.42) for the Information Sampling Task, number of boxes-opened and error scores, respectively, while the absolute measures of effect were 2.74 (95% CI 0.20, 5.28) and − 1.19 (95% CI -1.92, −0.46), respectively.
Working Memory Training
Two studies have tested computerized Working Memory Training versus sham training, one in cocaine and methamphetamine users (Bickel et al. 2011), and one in opioid users on methadone substitution therapy (Rass et al. 2015). Bickel et al. (2011) compared a progressive, voucher-incentive Working Memory Training with passive, non-incentive control (the program provided the correct answers to the cognitive exercises) using a yoked design, whereas Rass et al. (2015) compared a progressive, non-incentive Working Memory Training with active control (non-progressive working memory exercises) in a parallel-group RCT. Both studies used a broad battery of cognitive measures including hypothetical delay discounting, and risk-taking and reward-based decision-making (Balloon Analogue Risk Task and Iowa Gambling Task: Rass et al. 2015). Bickel et al. (2011) found significant time x treatment interaction effects on delay discounting, such that participants in the Working Memory Training condition significantly reduced discounting rates, compared to controls, after 25 days of training. The Hedges’s g were − 0.55 (95% CI -1.38, 0.27), −0.54 (95% CI -1.46, 0.39) and −0.57 (95% CI -1.37, 0.23) for the R100, H100 and H1000 k scores respectively, while the absolute measures of effect were −1.20 (95% CI -2.53, 0.13), −1.30 (95% CI -2.87, 0.27) and −1.20 (95% CI -2.69, 0.29), respectively. Conversely, Rass et al. (2015) did not find significant interaction effects of Working Memory Training on delay discounting or any other decision-making measures after similar exposure to training (25 sessions across 5 to 8 weeks). The Hedges’s g were − 0.03 (95% CI -0.11, 0.04) for the Hypothetical Delay Discounting Task and 0.18 (95% CI 0.11, 0.25) for the Quick Discounting Operant Task area under the curve scores, and 0.04 (95% CI -5.94, 6.02) for the Iowa Gambling Task score. The absolute measures of effect were − 0.01 (95% CI -0.14, 0.12) for the Hypothetical Delay Discounting Task and 0.05 (95% CI -0.08, 0.18) for the Quick Discounting Operant Task area under the curve scores, and 0.90 (95% CI -10.18, 11.98) for the Iowa Gambling Task score.
Cognitive Behavioral Therapy
Two studies have examined the effects of Cognitive Behavioral Therapy, one including participants with miscellaneous substance use disorders (Carroll et al. 2011) and one in participants with opioid use disorder (Tavakolian and Abolghasemi 2016). Carroll et al. (2011) tested the impact of 8 weeks of computer assisted Cognitive Behavioral Therapy versus TAU (a range of goal-directed change strategies), whereas Tavakolian and Abolghasemi (2016) compared the Meichenbaum Cognitive Restructuring Training (six 45 min sessions across 21 days) with no intervention in the context of opioid detoxification. Both studies randomized participants to treatment conditions and assessed an outcome relevant to decision-making using risk-taking (Balloon Analogue Risk Task: Carroll et al. 2011) and decision-making under uncertainty (Iowa Gambling Task: Tavakolian and Abolghasemi 2016). Tavakolian and Abolghasemi (2016) showed significant effects of the Meichenbaum training versus no intervention on decision-making in the Iowa Gambling Task, Hedges’s g = 0.77 (95% CI -2.93, 4.46) and absolute measure of effect = 7.86 (95% CI 2.07, 13.65). However, Carroll et al. (2011) did not find significant time x treatment interaction effects on risk-taking outcomes; data to calculate effect size was not available.
Contingency Management
Two studies compared Contingency Management plus Cognitive Behavioral Therapy with Cognitive Behavioral Therapy alone, one in participants with cannabis use disorder (Peters et al. 2013), and one in participants with tobacco use disorder (Weidberg et al. 2015). Peters et al. (2013) applied a 12 week treatment program and followed up participants after 12 months, while Weidberg et al. (2015) applied a six week program and assessed changes after treatment and at six months follow-up. Both studies randomized participants to treatment conditions, and used delay discounting measures as decision-making outcomes, experiential discounting task in Peters et al. (2013), and hypothetical discounting in Weidberg et al. (2015). Peters et al. (2013) found that participants enrolled in Cognitive Behavioral Therapy alone increased their delay discounting rates after 12 months (i.e., made more impulsive decisions), whereas those enrolled in Contingency Management plus Cognitive Behavioral Therapy maintained similar discounting rates, Hedges’s g = −1.07 (95% CI -1.25, −0.88) and absolute measure of effect = −0.96 (95% CI -1.39, 0.53). Weidberg et al. (2015) did not find a significant interaction effect on delay discounting after 6 week. However, they found a significant interaction between gender and treatment condition, meaning that women enrolled in Contingency Management plus Cognitive Behavioral Therapy showed greater reductions of delay discounting after 6 weeks of treatment, Hedges’s g effect size = 0.65 (95% CI -3.26, 4.56) and absolute measure of effect = 11.00 (95% CI 2.99, 19.01), and at six-month follow-up, Hedges’s g effect size = 0.24 (95% CI -3.67, 4.15) and absolute measure of effect = 4.00 (95% CI -3.81, 11.81).
Kiluk et al. (2017) compared 4 weeks of Contingency Management plus Cognitive Remediation Training versus Cognitive Remediation Training alone in a sample with miscellaneous substance use disorders. Cognitive Remediation Training included 12 sessions of attention, memory and problem solving exercises, and Contingency Management was paired with progress in the exercises. Participants were randomized to treatment conditions, and outcomes of interest included tasks of hypothetical delay discounting and risk-taking (Balloon Analogue Risk Task) among other more general cognitive indices. Results did not show significant interaction effects on the decision-making outcomes: Hedges’s g effect size = −0.06 (95% CI -4.42, 4.29) and absolute measure of effect = −0.90 (95% CI -7.97, 6.17) for Balloon Analogue Risk Task number of pumps, Hedges’s g effect size = 0.25 (−0.50, 1.00) and absolute measure of effect = 0.60 (95% CI -0.65, 1.85) for Balloon Analogue Risk Task popped balloons, and Hedges’s g effect size = −0.22 (95% CI -7.42, 6.98) and absolute measure of effect = −5.10 (95% CI -17.98, 7.78) for the delay discounting area under the curve. However, secondary analyses showed a moderating effect of attention exercises, meaning that participants enrolled in Contingency Management plus Cognitive Remediation Training that made more progress on attention exercises significantly reduced risk-taking after 4 weeks.
Other Interventions
Three other interventions have been tested in one study each. Black and Rosen (2011) examined the effects of the “Advisor-Teller Money Manager intervention,” which consists of goal-based strategies for money management, versus control (a budget workbook and similar contact with researchers) among participants with cocaine and alcohol use disorders. Participants were randomized to treatment conditions, and hypothetical delay discounting measured with the Monetary Choice Questionnaire (Kirby et al. 1999). Findings showed no significant effects of Advisor-Teller Money Manager versus control on delay discounting rates, data was not available for effect size calculations.
Two non-randomized proof of concept trials have examined the effects of innovative group interventions. Gonçalves et al. (2014) examined the effect of Chess training plus Motivational Interviewing, compared to active control (Motivational Interviewing and recreational activities), in participants with cocaine use disorder. The Chess training was aimed to improve cognitive control and planning abilities, while Motivational Interviewing was designed to generalize those skills to everyday life goals. Although the Chess plus Motivational Interviewing program had positive effects on attention skills after 4 weeks (10 sessions), it did not show significant effects on decision-making measured with the Iowa Gambling Task, Hedges’s g effect size = 0.05 (95% CI -0.18, 0.28) and absolute measure of effect = 0.04 (95% CI -0.75, 0.83). Finally, in the only study conducted in participants with Internet gaming disorder, Yao et al. (2017) examined the effect of Reality Therapy, which included planning strategies and mindfulness practice, versus no intervention in a healthy control group on measures of delay discounting (Monetary Choice Questionnaire) and risk-taking (Balloon Analogue Risk Task). Therapy sessions focused on self-monitoring strategies for impulsive behavior, and ended with a short mindfulness practice. After 6 weeks of training, participants enrolled in Reality Therapy showed significantly lower rates of delay discounting, Hedges’s g effect size = −0.77 (95% CI -0.94, −0.60) and absolute measure of effect = −0.41 (95% CI -0.71, −0.11), but no differences in risk-taking (Balloon Analogue Risk Task number of pumps), Hedges’s g effect size = −0.20 (95% CI -5.52, 5.11) and absolute measure of effect = −3.36 (−11.94, 5.22). Nonetheless, a secondary index of risk-taking in the Balloon Analogue Risk Task (popped balloons) showed a medium effect size, Hedges’s g = −0.59 (95% CI -1.75, 0.57) and absolute measure of effect = −2.12 (95% CI -4.55, 0.31), although this was mostly driven by increased risk-taking in the post- assessment of the control group.
Assessment of Risk Bias
The mean risk-of-bias across studies was 9.8 (SD = 1.6) on the Thompson et al. (2017) scale, which ranges from 0 to 13 (higher scores indicate less bias: Table 1). Detailed assessments are provided in Table S4 in the Supplementary Material. The main biases related to lack of standard RCT procedures, such as randomization, blinding and description of non-completers data.
Discussion
Consistent with our general hypothesis, we observed moderate (medium-large) beneficial effects of interventions directed at specific mechanisms of decision-making, such as Goal Management Training (cognitive control and emotional systems – the latter via mindfulness) and Contingency Management (reward system). The evidence was mixed for less specific interventions such as computerized Working Memory Training and Cognitive Behavioral Therapy, although the combination of these therapies with Contingency Management showed promising effects, and may partly explain the benefits of Contingency Management. Reality Therapy, including mindfulness practice, showed promising results in one trial, whereas Motivational Interview and Monetary Management had no beneficial effects on decision-making outcomes. Although risk-of-bias ratings were acceptable, the literature on this area is scarce, and dominated by pilot and proof of concept studies and secondary analyses of larger RCTs.
The moderate efficacy of Goal Management Training and Contingency Management may be explained by specificity to the neurocognitive systems of decision-making. Goal Management trains cognitive control using response inhibition and sustained attention exercises, and emotional awareness via mindfulness practice. After consolidating these skills, they are integrated in a concrete decision-making strategy (Stop – State goal – Check outcomes), which is practiced in real-life projects (Levine et al. 2011). These skills and strategies can promote a more cautious approach to decision-making (increased reflection) and boost representations of action-outcome relationships during decisions under uncertainty (Verdejo-García et al. 2018). Contingency Management focuses on retraining the reward system, with monetary payments replacing drug-related rewards, and community reinforcers promoting diversification of reward experiences versus drug-related sensitization or prioritization (Feldstein Ewing et al. 2011). This approach can reduce the appeal of reward-like signals in risk-taking tasks, and increase the value of non-drug, delayed rewards in delay discounting tasks (Shoptaw 2014). It is however important to consider that Goal Management Training and Contingency Management have been tested in the context of treatment as usual or concurrent interventions. Therefore, participants were more likely to be highly motivated and benefit from more general aspects of standard therapy (Gladwin et al. 2017). In the case of Contingency Management the combination with Cognitive Remediation or Cognitive Behavioral Therapy can also have additive or synergistic effects on the reward and cognitive control systems (Manning et al. 2017).
The beneficial effects of Goal Management Training and Contingency Management should not mask important biases. In the case of Goal Management Training, the two studies reviewed are from the same group, and one study was not randomized, which increases the risk of self-selection bias. There is yet another independent study that has shown beneficial effects of Goal Management Training on executive functions in people with methamphetamine use disorder, but it did not measure decision-making outcomes (Casaletto et al. 2016). In the case of Contingency Management, none of the studies showed a clear-cut superiority of Contingency Management versus control interventions. In two of the three Contingency Management trials beneficial effects were confined to specific subgroups, namely, women and participants with greater progress on concurrent attentional training (Kiluk et al. 2017; Weidberg et al. 2015), and in the third trial the time by treatment effects were partly attributable to deterioration in the control group (Peters et al. 2013). These considerations can be informative for subsequent trials, which should combine Contingency Management with other complementary interventions, such as cognitive remediation of attention or cognitive control, and take account of individual differences in therapeutic effects.
The mixed evidence for Working Memory Training and Cognitive Behavioral Therapy can be explained by important differences between studies. In the case of Working Memory Training, beneficial effects on decision-making were observed in a proof of concept study in stimulant users who received monetary incentives linked to training progress (Bickel et al. 2011), whereas no treatment effects were observed in an RCT in opioid users with no training-related incentives (Rass et al. 2015). The training programs used in these studies were also different (PSSCogReHab versus Cogmed), although both had similar exercises and active principles, such as adaptability, as well as comparable intensity. Since the PSSCogReHab program plus Contingency Management also had beneficial effects in the study by Kiluk et al. (2017), one possibility is that Working Memory Training, or cognitive training more generally, works better in the context of a concurrent incentive program due to additive effects on cognitive control and reward systems. Another possibility relates to differences in risk of bias, as the RCT design has greater experimental control and power.
In the case of Cognitive Behavioral Therapy, beneficial effects on decision-making were observed in a small pilot study using the Meichenbaum’s Cognitive Behavioral Therapy approach in opioid users (Tavakolian and Abolghasemi 2016), whereas no treatment effects were observed in secondary analyses of a larger RCT that tested the efficacy of computer-assisted Cognitive Behavioral Therapy in people with miscellaneous substance use disorders (Carroll et al. 2011). The studies also had different control groups, and it is possible that the superiority of the Meichembaum approach is due to comparison with no-intervention versus the more stringent comparison between computer-assisted Cognitive Behavioral Therapy and treatment as usual (van de Ven et al. 2016). These studies also differed in terms of risk of bias, with the study at lower risk yielding no beneficial effects (Carroll et al. 2011). However, neither of the two studies was well poised to yield definite conclusions, and more research is needed to establish if some forms of Cognitive Behavioral Therapy can have beneficial effects for decision-making skills in the context of addiction.
The beneficial effects of Reality Therapy on delay discounting among gamers will need replication in independent studies with adequate control groups. Some active ingredients of the therapy, such as planning and commitment, are well aligned with long-term based decision-making as measured by delay discounting measures (Crockett et al. 2013). However, the therapeutic focus on self-monitoring versus “hands on” exercises and the lack of integration of the mindfulness component, which was placed at the end of the sessions almost as a form of relaxation, make the approach too similar to non-specific interventions such as standard Cognitive Behavioral Therapy. In addition, since the control group was composed of healthy participants, improvement in the intervention group may be due to a regression to the mean effect. It is also unclear if beneficial effects could replicate in populations with more severe decision-making deficits, such as those with substance use and gambling disorders. Furthermore, current evidence does not support the usefulness of Motivational Interviewing or Monetary Management to improve decision-making skills. Null effects of Motivational Interviewing plus Chess training can be due to lack of specificity, as Motivational Interviewing deals with ambivalence and internal motivation for change, but not with the cognitive underpinnings of decision-making, whereas Chess training can stimulate cognitive control but not reward processing or emotional awareness. In the case of Monetary Management, the intervention may be too narrow to generalize to broader decision-making skills.
Intervention duration and individual variations in gender, age or abstinence can influence training effects on decision-making outcomes (Rezapour et al. 2016; Verdejo-Garcia 2016; Von Bastian and Oberauer 2014). Although we did not perform a quantitative analysis of the impact of these factors, a detailed inspection of studies designs and outcomes suggest that they did not play a major role in explaining the effects of the interventions. With regard to intervention duration, similar results were observed with shorter and longer versions of Contingency Management (4 to 12 weeks) and Goal Management Training (7 to 8 weeks). Moreover, in cases of discrepant findings (e.g., Working Memory Training), the shorter intervention (25 days in Bickel et al. 2011) achieved more beneficial effects that the longer intervention (5 to 8 weeks in Rass et al. 2015). With regard to individual variations, most of the studies imposed an age range (18 to 60 years) that minimizes age-related differences in decision-making (Mata et al. 2011), and matched the treatment and control groups on age. Baseline duration of abstinence was also generally well matched between treatment and comparison groups, although it is worth mentioning that several studies showing beneficial treatment effects included participants with at least 2 weeks and up to 12 months of abstinence pre-interventions, or were conducted in residential treatment settings, where it is more feasible to maintain and monitor abstinence (Alfonso et al. 2011; Bickel et al. 2011; Tavakolian and Abolghasemi 2016; Valls-Serrano et al. 2016). Therefore, an interesting question for future research is whether a particular duration of abstinence, and possibly abstinence-related recovery of basic cognitive skills, is a pre-requisite to benefit from decision-making interventions (Fernández-Serrano et al. 2011). Similar to the broad literature on addiction and cognition, most studies (7 out of 12) included only men or > 80% male participants. Therefore, we cannot draw overall conclusions about potential effects of gender differences on treatment response other than the discrete moderation effect reported by Weidberg et al. This is an important area for future research, as there is evidence for gender-related differences in decision-making skills (Bolla et al. 2004; van den Bos et al. 2013).
The results of this review also highlight important research needs in this area. Future research should focus on specific interventions for decision-making, and more rigorous RCTs that use decision-making tasks and clinical outcomes influenced by decision-making (e.g., relapse) as primary outcome measures. With regard to interventions, it seems reasonable to prioritize therapies that can address the multifaceted nature of decision-making, including reward, emotion and cognitive control. For example, it would be promising to test the effect of combining Contingency Management (reward) and Goal Management Training (emotion and cognitive control). An alternative strategy is to design new interventions that can address the three systems, and are tailored to people with addiction. In this context, it is interesting to speculate on how novel technologies, such as immersive technology or life-log technology, could help individuals to envisage and emotionally connect with the long-term consequences of hypothetical or real decisions. These technologies, in combination with “online” decision-making training, could help people with addiction to correct the short-term bias and strengthen the long-term focus of their decisions. With regard to methodological rigor, there is a need for more RCTs comparing the efficacy of decision-making interventions and adequate comparators matched on key methodological variables. Since decision-making interventions could be ultimately applied by psychologists, psychiatrists or occupational therapists that are already part of the addiction treatment workforce, these efficacy trials could be rapidly translated into more pragmatic trials and standard clinical practice. A useful asset for these trials would be a common suite of outcome measures. We have well-validated models and measures of decision-making, and hence it is feasible to achieve this harmonized suite through expert consensus, as it has been established for addiction treatment outcomes more generally (Donovan et al. 2012; Tiffany et al. 2012). Well-controlled RCTs and standardized outcome assessment would facilitate a systematic approach to the study of training-related and individual-related moderators of treatment effects (Von Bastian and Oberauer 2014).
In the interim, we tentatively conclude that specific neuropsychological and psychological interventions, such as Goal Management Training and Contingency Management, are promising strategies to improve decision-making among people with addiction in clinical settings. The evidence for the benefit of other therapies is tenuous. Moreover, research is scarce and dominated by small pilot and proof of concept studies, and secondary analyses of larger trials in which decision-making measures are not the primary outcomes. In addition, outcome measures vary across studies, which together with limited research preclude conclusions about specific components of decision-making. Given the significance of decision-making deficits in the context of addiction treatment, we advocate for more efficacy trials on promising intervention approaches, as well as a systematic approach to outcome assessment that collects comprehensive information on the different components of decision-making.
References
Alfonso, J. P., Caracuel, A., Delgado-Pastor, L. C., & Verdejo-García, A. (2011). Combined goal management training and mindfulness meditation improve executive functions and decision-making performance in abstinent polysubstance abusers. Drug and Alcohol Dependence, 117(1), 78–81.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Bechara, A. (2005). Decision making, impulse control and loss of willpower to resist drugs: A neurocognitive perspective. Nature Neuroscience, 8(11), 1458–1463.
Bechara, A., & Damasio, H. (2002). Decision-making and addiction (part I): Impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia, 40(10), 1675–1689.
Bechara, A., Tranel, D., & Damasio, H. (2000). Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain, 123(11), 2189–2202.
Bechara, A., Dolan, S., Denburg, N., Hindes, A., Anderson, S. W., & Nathan, P. E. (2001). Decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia, 39(4), 376–389.
Bechara, A., Dolan, S., & Hindes, A. (2002). Decision-making and addiction (part II): Myopia for the future or hypersensitivity to reward? Neuropsychologia, 40(10), 1690–1705.
Bickel, W. K., & Marsch, L. A. (2001). Toward a behavioral economic understanding of drug dependence: Delay discounting processes. Addiction, 96(1), 73–86.
Bickel, W. K., Yi, R., Landes, R. D., Hill, P. F., & Baxter, C. (2011). Remember the future: Working memory training decreases delay discounting among stimulant addicts. Biological Psychiatry, 69(3), 260–265.
Bickel, W. K., Moody, L., & Quisenberry, A. (2014). Computerized working-memory training as a candidate adjunctive treatment for addiction. Alcohol Research: Current Reviews, 36(1), 123–126.
Black, A. C., & Rosen, M. I. (2011). A money management-based substance use treatment increases valuation of future rewards. Addictive Behaviors, 36(1), 125–128.
Bolla, K. I., Eldreth, D. A., Matochik, J. A., & Cadet, J. L. (2004). Sex-related differences in a gambling task and its neurological correlates. Cerebral Cortex, 14(11), 1226–1232.
Brand, M., Labudda, K., & Markowitsch, H. J. (2006). Neuropsychological correlates of decision-making in ambiguous and risky situations. Neural Networks, 19(8), 1266–1276.
Carroll, K. M., Kiluk, B. D., Nich, C., Babuscio, T. A., Brewer, J. A., Potenza, M. N., Ball, S. A., Martino, S., Rounsaville, B. J., & Lejuez, C. W. (2011). Cognitive function and treatment response in a randomized clinical trial of computer-based training in cognitive-behavioral therapy. Substance Use & Misuse, 46(1), 23–34.
Casaletto, K. B., Moore, D. J., Woods, S. P., Umlauf, A., Scott, J., & Heaton, R. K. (2016). Abbreviated goal management training shows preliminary evidence as a neurorehabilitation tool for HIV-associated neurocognitive disorders among substance users. The Clinical Neuropsychologist, 30(1), 107–130.
Clark, L., Robbins, T. W., Ersche, K. D., & Sahakian, B. J. (2006). Reflection impulsivity in current and former substance users. Biological Psychiatry, 60(5), 515–522.
Crockett, M. J., Braams, B. R., Clark, L., Tobler, P. N., Robbins, T. W., & Kalenscher, T. (2013). Restricting temptations: Neural mechanisms of precommitment. Neuron, 79(2), 391–401.
Daw, N. D., Gershman, S. J., Seymour, B., Dayan, P., & Dolan, R. J. (2011). Model-based influences on humans' choices and striatal prediction errors. Neuron, 69(6), 1204–1215.
Donovan, D. M., Bigelow, G. E., Brigham, G. S., Carroll, K. M., Cohen, A. J., Gardin, J. G., Hamilton, J. A., Huestis, M. A., Hughes, J. R., Lindblad, R., Marlatt, G. A., Preston, K. L., Selzer, J. A., Somoza, E. C., Wakim, P. G., & Wells, E. A. (2012). Primary outcome indices in illicit drug dependence treatment research: Systematic approach to selection and measurement of drug use end-points in clinical trials. Addiction, 107(4), 694–708.
Feldstein Ewing, S. W., Filbey, F. M., Hendershot, C. S., McEachern, A. D., & Hutchison, K. E. (2011). Proposed model of the neurobiological mechanisms underlying psychosocial alcohol interventions: The example of motivational interviewing. Journal of Studies on Alcohol and Drugs, 72(6), 903–916.
Fernández-Serrano, M. J., Pérez-García, M., & Verdejo-García, A. (2011). What are the specific vs. generalized effects of drugs of abuse on neuropsychological performance? Neuroscience & Biobehavioral Reviews, 35(3), 377–406.
Fu, R., Vandermeer, B. W., Shamliyan, T. A., O’Neil, M. E., Yazdi, F., Fox, S. H., Morton, S. C. (2013). Handling continuous outcomes in quantitative synthesis. Methods guide for comparative effectiveness reviews. AHRQ Publication No. 13-EHC103-EF. Rockville, MD: Agency for Healthcare Research and Quality.
Gladwin, T. E., Wiers, C. E., & Wiers, R. W. (2017). Interventions aimed at automatic processes in addiction: Considering necessary conditions for efficacy. Current Opinion in Behavioral Sciences, 13, 19–24.
Gonçalves, P. D., Ometto, M., Bechara, A., Malbergier, A., Amaral, R., Nicastri, S., Martins, P. A., Beraldo, L., dos Santos, B., Fuentes, D., Andrade, A. G., Busatto, G. F., & Cunha, P. J. (2014). Motivational interviewing combined with chess accelerates improvement in executive functions in cocaine dependent patients: A one-month prospective study. Drug and Alcohol Dependence, 141, 79–84.
Goudriaan, A. E., Oosterlaan, J., de Beurs, E., & van den Brink, W. (2005). Decision making in pathological gambling: A comparison between pathological gamblers, alcohol dependents, persons with Tourette syndrome, and normal controls. Cognitive Brain Research, 23(1), 137–151.
Grant, S., Contoreggi, C., & London, E. D. (2000). Drug abusers show impaired performance in a laboratory test of decision making. Neuropsychologia, 38(8), 1180–1187.
Heyman, G. M. (2009). Addiction: A disorder of choice: Harvard University Press.
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., Savovic, J., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ, 343(oct18 2), d5928.
Holt, D. D., Green, L., & Myerson, J. (2012). Estimating the subjective value of future rewards: Comparison of adjusting-amount and adjusting-delay procedures. Behavioural Processes, 90(3), 302–310.
Huntley, J. D., Gould, R. L., Liu, K., Smith, M., & Howard, R. J. (2015). Do cognitive interventions improve general cognition in dementia? A meta-analysis and meta-regression. BMJ Open, 5(4), e005247. https://doi.org/10.1136/bmjopen-2014-005247.
Johnson, M. W., Bickel, W. K., & Baker, F. (2007). Moderate drug use and delay discounting: A comparison of heavy, light, and never smokers. Experimental and Clinical Psychopharmacology, 15(2), 187–194.
Kiluk, B. D., Buck, M. B., Devore, K. A., Babuscio, T. A., Nich, C., & Carroll, K. M. (2017). Performance-based contingency management in cognitive remediation training: A pilot study. Journal of Substance Abuse Treatment, 72, 80–88.
Kirby, K. N., Petry, N. M., & Bickel, W. K. (1999). Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General, 128(1), 78–87.
Lejuez, C. W., Read, J. P., Kahler, C. W., Richards, J. B., Ramsey, S. E., Stuart, G. L., Strong, D. R., & Brown, R. A. (2002). Evaluation of a behavioral measure of risk taking: The balloon analogue risk task (BART). Journal of Experimental Psychology: Applied, 8(2), 75–84.
Levine, B., Stuss, D. T., Winocur, G., Binns, M. A., Fahy, L., Mandic, M., Bridges, K., & Robertson, I. H. (2007). Cognitive rehabilitation in the elderly: Effects on strategic behavior in relation to goal management. Journal of the International Neuropsychological Society, 13(1), 143–152.
Levine, B., Schweizer, T. A., O'Connor, C., Turner, G., Gillingham, S., Stuss, D. T., Manly, T., & Robertson, I. H. (2011). Rehabilitation of executive functioning in patients with frontal lobe brain damage with goal management training. Frontiers in Human Neuroscience, 5.
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., Clarke, M., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ, 339(jul21 1), b2700.
Manning, V., Verdejo-Garcia, A., & Lubman, D. I. (2017). Neurocognitive impairment in addiction and opportunities for intervention. Current Opinion in Behavioral Sciences, 13, 40–45.
Mata, R., Josef, A. K., Samanez-Larkin, G. R., & Hertwig, R. (2011). Age differences in risky choice: A meta-analysis. Annals of the New York Academy of Sciences, 1235(1), 18–29.
Morris, S. B. (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods, 11(2), 364–386.
Noël, X., Brevers, D., & Bechara, A. (2013). A neurocognitive approach to understanding the neurobiology of addiction. Current Opinion in Neurobiology, 23(4), 632–638.
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan-a web and mobile app for systematic reviews. Systematic reviews, 5(1), 210.
Peters, E. N., Petry, N. M., LaPaglia, D. M., Reynolds, B., & Carroll, K. M. (2013). Delay discounting in adults receiving treatment for marijuana dependence. Experimental and Clinical Psychopharmacology, 21(1), 46–54.
Rass, O., Schacht, R. L., Buckheit, K., Johnson, M. W., Strain, E. C., & Mintzer, M. Z. (2015). A randomized controlled trial of the effects of working memory training in methadone maintenance patients. Drug and Alcohol Dependence, 156, 38–46.
Redish, A. D., Jensen, S., & Johnson, A. (2008). Addiction as vulnerabilities in the decision process. Behavioral and Brain Sciences, 31(4), 461–487.
Reynolds, B., & Schiffbauer, R. (2004). Measuring state changes in human delay discounting: An experiential discounting task. Behavioural Processes, 67(3), 343–356.
Rezapour, T., DeVito, E. E., Sofuoglu, M., & Ekhtiari, H. (2016). Perspectives on neurocognitive rehabilitation as an adjunct treatment for addictive disorders: From cognitive improvement to relapse prevention. Progress in Brain Research, 224, 345–369.
Robinson, T. E., & Berridge, K. C. (2008). The incentive sensitization theory of addiction: Some current issues. Philosophical Transactions of the Royal Society of London B: Biological Sciences, 363(1507), 3137–3146.
Schiebener, J., & Brand, M. (2015). Decision making under objective risk conditions–a review of cognitive and emotional correlates, strategies, feedback processing, and external influences. Neuropsychology Review, 25(2), 171–198.
Shoptaw, S. (2014). Commentary on Gowin et al.(2014): Brain is behavior—Methamphetamine dependence and recovery. Addiction, 109(2), 248–249.
Stanger, C., Budney, A. J., & Bickel, W. K. (2013). A developmental perspective on neuroeconomic mechanisms of contingency management. Psychology of Addictive Behaviors, 27(2), 403–415.
Stevens, L., Goudriaan, A., Verdejo-Garcia, A., Dom, G., Roeyers, H., & Vanderplasschen, W. (2015). Impulsive choice predicts short-term relapse in substance-dependent individuals attending an in-patient detoxification programme. Psychological Medicine, 45(10), 2083–2093.
Stewart, J. L., Flagan, T. M., May, A. C., Reske, M., Simmons, A. N., & Paulus, M. P. (2013). Young adults at risk for stimulant dependence show reward dysfunction during reinforcement-based decision making. Biological Psychiatry, 73(3), 235–241.
Stewart, J. L., Butt, M., May, A. C., Tapert, S. F., & Paulus, M. P. (2017). Insular and cingulate attenuation during decision making is associated with future transition to stimulant use disorder. Addiction, 112(9), 1567–1577.
Tavakolian, E., & Abolghasemi, A. (2016). Effects of cognitive restructuring training on neurocognitive functions in opioid addicts. Archives of Psychiatry and Psychotherapy, 18(1), 14–21.
Thompson, T., Oram, C., Correll, C. U., Tsermentseli, S., & Stubbs, B. (2017). Analgesic effects of alcohol: A systematic review and meta-analysis of controlled experimental studies in healthy participants. The Journal of Pain, 18(5), 499–510.
Tiffany, S. T., Friedman, L., Greenfield, S. F., Hasin, D. S., & Jackson, R. (2012). Beyond drug use: A systematic consideration of other outcomes in evaluations of treatments for substance use disorders. Addiction, 107(4), 709–718.
Valls-Serrano, C., Caracuel, A., & Verdejo-Garcia, A. (2016). Goal management training and mindfulness meditation improve executive functions and transfer to ecological tasks of daily life in polysubstance users enrolled in therapeutic community treatment. Drug and Alcohol Dependence, 165, 9–14.
van de Ven, R. M., Murre, J. M., Veltman, D. J., & Schmand, B. A. (2016). Computer-based cognitive training for executive functions after stroke: A systematic review. Frontiers in Human Neuroscience, 10.
van den Bos, R., Homberg, J., & de Visser, L. (2013). A critical review of sex differences in decision-making tasks: Focus on the Iowa gambling task. Behavioural Brain Research, 238, 95–108.
Verdejo-Garcia, A. (2016). Cognitive training for substance use disorders: Neuroscientific mechanisms. Neuroscience and Biobehavioral Reviews, 68, 270–281.
Verdejo-García, A., & Bechara, A. (2009). A somatic marker theory of addiction. Neuropharmacology, 56, 48–62.
Verdejo-Garcia, A., Albein-Urios, N., Martinez-Gonzalez, J. M., Civit, E., De la Torre, R., & Lozano, O. (2014). Decision-making impairment predicts 3-month hair-indexed cocaine relapse. Psychopharmacology, 231(21), 4179–4187.
Verdejo-García, A., Chong, T. T.-J., Stout, J. C., Yücel, M., & London, E. D. (2018). Stages of dysfunctional decision-making in addiction. Pharmacology Biochemistry and Behavior, 164, 99–105.
von Bastian, C. C., & Oberauer, K. (2014). Effects and mechanisms of working memory training: A review. Psychological Research, 78(6), 803–820.
Weidberg, S., Landes, R. D., García-Rodríguez, O., Yoon, J. H., & Secades-Villa, R. (2015). Interaction effect of contingency management and sex on delay-discounting changes among treatment-seeking smokers. Experimental and Clinical Psychopharmacology, 23(5), 361–368.
Wesley, M. J., & Bickel, W. K. (2014). Remember the future II: Meta-analyses and functional overlap of working memory and delay discounting. Biological Psychiatry, 75(6), 435–448.
World Health Organisation (2016). ICD-11 Beta Draft: International Classification of Diseases. https://icd.who.int/dev11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f1448597234.
Yao, Y.-W., Chen, P.-R., Chiang-shan, R. L., Hare, T. A., Li, S., Zhang, J.-T., et al. (2017). Combined reality therapy and mindfulness meditation decrease intertemporal decisional impulsivity in young adults with internet gaming disorder. Computers in Human Behavior, 68, 210–216.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(DOCX 35 kb)
Rights and permissions
About this article
Cite this article
Verdejo-García, A., Alcázar-Córcoles, M.A. & Albein-Urios, N. Neuropsychological Interventions for Decision-Making in Addiction: a Systematic Review. Neuropsychol Rev 29, 79–92 (2019). https://doi.org/10.1007/s11065-018-9384-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-018-9384-6