Abstract
This study compared patterns of prenatal care among mothers who used methamphetamine (MA) during pregnancy and non-using mothers in the US and New Zealand (NZ), and evaluated associations among maternal drug use, child protective services (CPS) referral, and inadequate prenatal care in both countries. The sample consisted of 182 mothers in the MA-Exposed and 196 in the Comparison groups in the US, and 107 mothers in the MA-Exposed and 112 in the Comparison groups in NZ. Positive toxicology results and/or maternal report of MA use during pregnancy were used to identify MA use. Information about sociodemographics, prenatal care and prenatal substance use was collected by maternal interview. MA-use during pregnancy is associated with lower socioeconomic status, single marital status, and CPS referral in both NZ and the US. Compared to their non-using counterparts, MA-using mothers in the US had significantly higher rates of inadequate prenatal care. No association was found between inadequate care and MA-use in NZ. In the US, inadequate prenatal care was associated with CPS referral, but not in NZ. Referral to CPS for drug use only composed 40 % of all referrals in the US, but only 15 % of referrals in NZ. In our study population, prenatal MA-use and CPS referral eclipse maternal sociodemographics in explanatory power for inadequate prenatal care. The predominant effect of CPS referral in the US is especially interesting, and should encourage further research on whether the US policy of mandatory reporting discourages drug-using mothers from seeking antenatal care.

Similar content being viewed by others
References
Lagasse L. L., Wouldes T., Newman E., et al. (2010). Prenatal methamphetamine exposure and neonatal neurobehavioral outcome in the USA and New Zealand. Neurotoxicology and Teratology, 33(1), 166–175.
Gonzales, R., Mooney, L., & Rawson, R. A. (2010). The methamphetamine problem in the United States. Annual Review of Public Health, 31, 385–398.
Watanabe-Galloway, S., Ryan, S., Hansen, K., et al. (2009). Effects of methamphetamine abuse beyond individual users. Journal of Psychoactive Drugs, 41(3), 241–248.
McKetin, R., Kozel, N., Douglas, J., et al. (2008). The rise of methamphetamine in Southeast and East Asia. Drug and Alcohol Review, 27(3), 220–228.
Crime UNOoDa. (2007). World Drug Report 2007. New York: United Nations Publications 2007.
Terplan, M., Smith, E. J., Kozloski, M. J., et al. (2009). Methamphetamine use among pregnant women. Obstetrics and Gynecology, 113(6), 1285–1291.
Arria, A. M., Derauf, C., Lagasse, L. L., et al. (2006). Methamphetamine and other substance use during pregnancy: Preliminary estimates from the Infant Development, Environment, and Lifestyle (Ideal) Study. Maternal and Child Health Journal, 10(3), 293–302.
Wilkins, C., Bhatta, K., & Casswell, S. (2002). The emergence of amphetamine use in New Zealand: Findings from the 1998 and 2001 national drug surveys. The New Zealand Medical Journal, 115(1166), U256.
Wilkins, C., & Sweetsur, P. (2008). Trends in population drug use in New Zealand: Findings from National Household Surveying of Drug Use in 1998, 2001, 2003, and 2006. The New Zealand Medical Journal, 121(1274), 61–71.
Wouldes, T., LaGasse, L., Sheridan, J., et al. (2004). Maternal methamphetamine use during pregnancy and child outcome: What do we know? The New Zealand Medical Journal, 117(1206), U1180.
Brady, T. M., Visscher, W., Feder, M., et al. (2003). Maternal drug use and the timing of prenatal care. Journal of Health Care for the Poor and Underserved, 14(4), 588–607.
Shieh, C., & Kravitz, M. (2006). Severity of drug use, initiation of prenatal care, and maternal-fetal attachment in pregnant marijuana and cocaine/heroin users. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 35(4), 499–508.
Minnes, S., Singer, L. T., Humphrey-Wall, R., et al. (2008). Psychosocial and behavioral factors related to the post-partum placements of infants born to cocaine-using women. Child Abuse and Neglect, 32(3), 353–366.
Berenson, A. B., Wilkinson, G. S., & Lopez, L. A. (1996). Effects of prenatal care on neonates born to drug-using women. Substance Use and Misuse, 31(8), 1063–1076.
Burkett, G., Gomez-Marin, O., Yasin, S. Y., et al. (1998). Prenatal care in cocaine-exposed pregnancies. Obstetrics and Gynecology, 92(2), 193–200.
El-Mohandes, A., Herman, A. A., Nabil El-Khorazaty, M., et al. (2003). Prenatal care reduces the impact of illicit drug use on perinatal outcomes. Journal of Perinatology, 23(5), 354–360.
MacGregor, S. N., Keith, L. G., Bachicha, J. A., et al. (1989). Cocaine abuse during pregnancy: Correlation between prenatal care and perinatal outcome. Obstetrics and Gynecology, 74(6), 882–885.
Quinlivan, J. A., & Evans, S. F. (2002). The impact of continuing illegal drug use on teenage pregnancy outcomes–a prospective cohort study. British Journal of Obstetrics and Gynaecology, 109(10), 1148–1153.
Racine, A., Joyce, T., & Anderson, R. (1993). The association between prenatal care and birth weight among women exposed to cocaine in New York City. Journal of the American Medical Association, 270(13), 1581–1586.
Chazotte, C., Youchah, J., & Freda, M. C. (1995). Cocaine using during pregnancy and low birth weight: The impact of prenatal care and drug treatment. Seminars in Perinatology, 19(4), 293–300.
Poland, M. L., Dombrowski, M. P., Ager, J. W., et al. (1993). Punishing pregnant drug users: enhancing the flight from care. Drug and Alcohol Dependence, 31(3), 199–203.
Downe, S., Finlayson, K., Walsh, D., et al. (2009). ‘Weighing up and balancing out’: A meta-synthesis of barriers to antenatal care for marginalised women in high-income countries. British Journal of Obstetrics and Gynaecology, 116(4), 518–529.
Grandy, M. C. T., Duerden, J., Mannion, K. (2002). Drug misuse in pregnancy in the Northern and Yorkshire region. In: Northern and Yorkshire Public Health Observatory WRI, University of Durham Queen’s Campus, University of Boulevard, Stockton on Tees editor.
Milligan, R., Wingrove, B. K., Richards, L., et al. (2002). Perceptions about prenatal care: Views of urban vulnerable groups. BMC Public Health, 2, 25.
Reis, J., Mills-Thomas, B., Robinson, D., et al. (1992). An inner-city community’s perspective on infant mortality and prenatal care. Public Health Nursing, 9(4), 248–256.
Roberts, S., Pies, C. (2011). Complex calculations: How drug use during pregnancy becomes a barrier to prenatal care. Maternal and Child Health Journal, 15(3), 333–341.
Roberts, S. C. M. (2009). Re-contextualizing universal screening for alcohol and drug use in prenatal care: The (not so) hidden connections between universal screening and reporting to child protective services. Berkeley, CA: University of California, Berkeley.
Roberts, S. C. M., Nuru-Jeter, A. (2010). Women’s perspectives on screening for alcohol and drug use in prenatal care. Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health, 20(3), 193–200.
Schempf, A. H., Strobino, D. M. (2009). Drug use and limited prenatal care: An examination of responsible barriers. American Journal of Obstetrics and Gynecology, 200(4), 412.e1–412.e10.
Lester, B. M., Andreozzi, L., & Appiah, L. (2004). Substance use during pregnancy: Time for policy to catch up with research. Harm Reduction Journal, 1(1), 5.
Della Grotta, S., LaGasse, L., Arria, A., et al. (2010). Patterns of methamphetamine use during pregnancy: Results from the Infant Development, Environment, and Lifestyle (IDEAL) Study. Maternal and Child Health Journal, 14(4), 519–27.
Institute of Medicine, National Academy of Sciences, (1974). Infant deaths, an analysis by maternal risk and health care. In: Contrasts in health status, Vol. I, 1973. Based on: The American College of Obstetricians and Gynecologists: Standards for Obstetric-Gynecologic Services. Chicago.
Johnson, A. A., El-Khorazaty, M. N., Hatcher, B. J., et al. (2003). Determinants of late prenatal care initiation by African American women in Washington. Dc. Maternal and Child Health Journal, 7(2), 103–114.
Funkhouser, A. W., Butz, A. M., Feng, T. I., et al. (1993). Prenatal care and drug use in pregnant women. Drug and Alcohol Dependence, 33(1), 1–9.
Melnikow, J., Alemagno, S. A., Rottman, C., et al. (1991). Characteristics of inner-city women giving birth with little or no prenatal care: A case-control study. Journal of Family Practice, 32(3), 283−286.
Kalmuss, D., Fennelly, K. (1990). Barriers to prenatal care among low-income women in New York City. Family Planning Perspectives, 22(5), 215–218, 231.
Maupin, J. R., Lyman, R., Fatsis, J., et al. (2004). Characteristics of women who deliver with no prenatal care. Journal of Maternal-Fetal and Neonatal Medicine, 16(1), 45–50.
Pagnini, D. L., & Reichman, N. E. (2000). Psychosocial factors and the timing of prenatal care among women in New Jersey’s healthstart program. Family Planning Perspectives, 32(2), 56–64.
Melnikow, J., Alemagno, S. (1993). Adequacy of prenatal care among inner-city women. Journal of Family Practice, 37(6), 575–578.
Funai, E. F., White, J., Lee, M. J., et al. (2003). Compliance with prenatal care visits in substance abusers. Journal of Maternal-Fetal and Neonatal Medicine, 14, 329–332.
Shankaran, S., Bauer, C. R., Bada, H. S., et al. (2003). Health-care utilization among mothers and infants following cocaine exposure. Journal of Perinatology, 23(5), 361–367.
Scupholme, A., Robertson, E. G., & Kamons, A. S. (1991). Barriers to prenatal care in a multiethnic, urban sample. Journal of Nurse-Midwifery, 36(2), 111–116.
Hoffman, C., & Paradise, J. (2008). Health insurance and access to health care in the United States. Annals of the New York Academy of Sciences, 1136(1), 149–160.
Marquis, M. S., & Long, S. H. (2002). The role of public insurance and the public delivery system in improving birth outcomes for low-income pregnant women. Medical Care, 40(11), 1048–1059.
Nothnagle, M., Marchi, K., Egerter, S., et al. (2000). Risk factors for late or no prenatal care following medicaid expansions in California. Maternal and Child Health Journal, 4(4), 251–259.
Cooney, J. P. (1985). What determines the start of prenatal care? Prenatal care, insurance, and education. Medical Care, 23(8), 986–997.
Oberg, C. N., Lia-Hoagberg, B., Hodkinson, E., et al. (1990). Prenatal care comparisons among privately insured, uninsured, and medicaid-enrolled women. Public Health Reports, 105(5), 533–535.
Brown, S. (Ed.). (1988). Prenatal care: Reaching mothers, reaching infants. Washington, DC: Institute of Medicine/National Academy Press.
Hadley, J. (2003). Sicker and poorer: The consequences of being uninsured: A review of the research on the relationship between health insurance, medical care use, health, work, and income. Medical Care Research and Review, 60(2 suppl), 3S–75S.
Joseph, C. L. (1989). Identification of factors associated with delayed antenatal care. Journal of the National Medical Association, 81(1), 57–63.
McQuide, P. A., Delvaux, T., Buekens, P., et al. (1998). Prenatal care incentives in Europe. Journal of Public Health Policy, 19(3), 331–349.
Bueche, M. N. (1990). Maternal-infant health care: A comparison between the United States and West Germany. Nursing Forum, 25(4), 26–30.
Buekens, P., Kotelchuck, M., Blondel, B., et al. (1993). A comparison of prenatal care use in the United States and Europe. American Journal of Public Health, 83(1), 31–36.
Williams, B. C. (1994). Social approaches to lowering infant mortality: Lessons from the European experience. Journal of Public Health Policy, 15(1), 18–25.
Miller, C. A. (1987). Matemal health and infant survival. Washington DC: National Center for Clinical Infant Programs.
Beeckman, K., Louckx, F., Putman, K. (2011). Predisposing, enabling and pregnancy-related determinants of late initiation of prenatal care. Maternal and Child Health Journal, 15(7), 1067–1075.
Blondel, B., & Marshall, B. (1998). Poor antenatal care in 20 French districts: Risk factors and pregnancy outcome. Journal of Epidemiology and Community Health, 52(8), 501–506.
Lia-Hoagberg, B., Rode, P., Skovholt, C. J., et al. (1990). Barriers and motivators to prenatal care among low-income women. Social Science and Medicine, 30(4), 487–494.
McDonald, T. P., Coburnm, A. F. (1988). Predictors of prenatal care utilization. Social Science and Medicine (1982), 27(2), 167–172.
St Clair, P. A., Smeriglio, V. L., Alexander, C. S., et al. (1990). Situational and financial barriers to prenatal care in a sample of low-income, inner-city women. Public Health Reports, 105(3), 264–267.
Braveman, P., Bennett, T., Lewis, C., et al. (1993). Access to prenatal care following major medicaid eligibility expansions. Journal of the American Medical Association, 269(10), 1285–1289.
Haas, J. S., Udvarhelyi, I. S., Morris, C. N., et al. (1993). The effect of providing health coverage to poor uninsured pregnant women in Massachusetts. Journal of the American Medical Association, 269(1), 87–91.
Piper, J. M., Ray, W. A., & Griffin, M. R. (1990). Effects of medicaid eligibility expansion on prenatal care and pregnancy outcome in Tennessee. Journal of the American Medical Association, 264(17), 2219–2223.
Parchment, W., Weiss, G., & Passannante, M. R. (1996). Is the lack of health insurance the major barrier to early prenatal care at an inner-city hospital? Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health, 6(2), 97–105.
Braveman, P., Marchi, K., Egerter, S., et al. (2000) Barriers to timely prenatal care among women with insurance: The importance of prepregnancy factors. Obstetrics and Gynecology, 95(6, Part 1), 874–880.
Braveman, P. A., Egerter, S. A., Cubbin, C., et al. (2004). An approach to studying social disparities in health and health care. American Journal of Public Health, 94(12), 2139–2148.
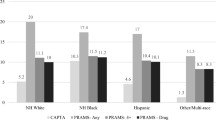
Frisbie, W. P., Echevarria, S., & Hummer, R. A. (2001). Prenatal care utilization among non-Hispanic Whites, African Americans, and Mexican Americans. Maternal and Child Health Journal, 5(1), 21–33.
Goldenberg, R. L., Patterson, E. T., & Freese, M. P. (1992). Maternal demographic, situational and psychosocial factors and their relationship to enrollment in prenatal care: A review of the literature. Women and Health, 19(2–3), 133–151.
Mathews, B., & Kenny, M. C. (2008). Mandatory reporting legislation in the United States, Canada, and Australia: A cross-jurisdictional review of key features, differences, and issues. Child Maltreatment, 13(1), 50–63.
Gateway, C. W. I. (2009). Definitions of child abuse and neglect: Summary of state laws. Washington, DC: U.S. Department of Health and Human Services Administration for Children and Families, Children’s Bureau.
Lester, B. M., & Twomey, J. E. (2007). Treatment of substance abuse during pregnancy. Women’s Health, 4(1), 67–77.
Campbell, D. E., & Fleischman, A. R. (1992). Ethical challenges in medical care for the pregnant substance abuser. Clinical Obstetrics and Gynecology, 35(4), 803–812.
Rubenstein, L. (1991). Prosecuting maternal substance abusers: An unjustified and ineffective policy. Yale Law and Policy Review, 9(1), 130–160.
Coleman, E., & Miller, M. K. (2006). Assessing legal responses to prenatal drug use: Can therapeutic responses produce more positive outcomes than punitive responses. Journal of Law and Health, 20(35), 35–67.
Barth, R. P. (2001). Research outcomes of prenatal substance exposure and the need to review policies and procedures regarding child abuse reporting. Child Welfare, 80(2), 275–296.
Madden, R. G. (1993). State actions to control fetal abuse: Ramifications for child welfare practice. Child Welfare, 72(2), 129–140.
Acknowledgments
The official name of the project is Prenatal Methamphetamine Exposure and Child Development in New Zealand and USA. This study was supported by a grant from the National Institute on Drug Abuse (Grant #R01DA021757) and a US Graduate Student grant from the Fulbright New Zealand Programme. We thank Carolyn Ho, Jenny Rogers, Jo Cliffe, Sue Cumming, Gillian Gee, Christine Todd, and Heather Stewart in Auckland, New Zealand for their assistance in this international collaboration.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, M., LaGasse, L.L., Wouldes, T.A. et al. Predictors of Inadequate Prenatal Care in Methamphetamine-Using Mothers in New Zealand and the United States. Matern Child Health J 17, 566–575 (2013). https://doi.org/10.1007/s10995-012-1033-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-012-1033-8