Abstract
Purpose
To evaluate the utility of a telephone outcall program for cancer caregivers and to examine longitudinal changes in their distress levels and supportive care needs.
Methods
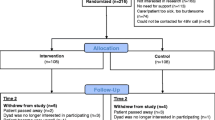
As part of the PROTECT trial, caregivers assigned to the intervention arm (N = 108) received three telephone outcalls from a Cancer Council 13 11 20 nurse at three time points (7–10 days post-randomization, 1 and 4 months later). During each call, caregivers were screened for distress using the Distress Thermometer (range: 0–10) then six supportive care issues were raised for discussion. Participants completed a utility survey 1 month post-intervention.
Results
The outcall program was highly acceptable and perceived as beneficial by caregivers. Overall, 95% reported it was worth their time to take part in the outcall program and 82% stated that the program was very relevant to them. Level of distress and impact of distress decreased over time (p = 0.0031, p < 0.0001, respectively). Average call duration decreased over time (p < 0.0001) and was longer for female than male caregivers (p = 0.0009). The frequency of caregivers discussing issues related to psychological distress (p = 0.0003), health literacy (p < 0.0001), financial (p = 0.0014), and practical concerns (p = 0.0121) decreased over time. Psychological distress was more often discussed by female than male caregivers (p = 0.0153), and family issues more often by younger (< 55 years) than older caregivers (p = 0.0071).
Conclusions
Utility of this outcall program was high. Caregivers’ level of distress and unmet needs decreased over time. Gender and age differences emerged, which warrants the need for tailored support. Further research is necessary to identify the best method of improving access to 13 11 20 services for caregivers.


Similar content being viewed by others
References
Northouse LL, Katapodi MC, Schafenacker AM, Weiss D (2012) The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Semin Psyc Nurs 28:236–245
Tamayo GJ, Broxson A, Munsell M, Cohen MZ (2010) Caring for the caregiver. Oncol Nurs Forum 37:E50–E57
Lambert SD, Girgis A, Lecathelinais C, Stacey F (2013) Walking a mile in their shoes: anxiety and depression among partners and caregivers of cancer survivors at 6 and 12 months post-diagnosis. Support Care Cancer 21:75–85
Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS (2014) Caregiver burden: a clinical review. JAMA 311:1052–1059
Van Ryn M, Sanders S, Kahn K, van Houtven C, Griffin JM, Martin M et al (2011) Objective burden, resources, and other stressors among informal cancer caregivers: a hidden quality issue? Psycho-Oncology 20:44–52
Stenberg U, Ruland CM, Miaskowski C (2010) Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology 19:1013–1025
Ockerby C, Livingston P, O’Connell B, Gaskin CJ (2013) The role of informal caregivers during cancer patients’ recovery from chemotherapy. Scand J Caring Sci 27:147–155
Given BA, Given CW, Sherwood P (2012) The challenge of quality cancer care for family caregivers. Semin Oncol Nurs 28:205–212
Girgis A, Lambert SD, McElduff P, Bonevski B, Lecathelinais C, Boyes A, Stacey F (2013) Some things change, some things stay the same: a longitudinal analysis of cancer caregivers’ unmet supportive care needs. Psycho-Oncology 22:1557–1564
Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, Willan A, Viola R, Coristine M, Janz T, Glossop R (2004) Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ 170:1795–1801
Kim Y, Kashy DA, Spillers RL, Evans TV (2010) Needs assessment of family caregivers of cancer survivors: three cohort comparison. Psycho-Oncology 19:573–582
Lambert SD, Harrison JD, Smith E, Bonevski B, Carey M, Lawsin C, Paul C, Girgis A (2012) The unmet needs of partners and caregivers of adults diagnosed with cancer: a systematic review. BMJ Support Palliat Care 2:224–230
Heckel L, Fennell KM, Reynolds J, Osborne RH, Chirgwin J, Botti M, Ashley DM, Livingston PM (2015) Unmet needs and depression among carers of people newly diagnosed with cancer. EJC 51:2049–2057
American College of Surgeons (ACS) (2015) Cancer program standards: ensuring patient-centered care. American College of Surgeons, Chicago IL
Chiang A (2016) Assessing emotional distress in patients with cancer. Proc Am Soc Clin Oncol 2015 https://am.asco.org/assessing-emotional-distress-patients-cancer. Accessed 22 November 2016
Kramar A, Gandee M, Marino MJ, Patton A, Kendall J, McMullen L et al (2015) Psycho-social distress screening. Lessons learned from three ACCC member programs, Association of Community Cancer Centres (ACCC), Rockville MD
National Comprehensive Cancer Network (NCCN) (2003) Distress management clinical practice guidelines. JCCN 1:344–374
Trad W, Koh E-S, Daher M, Bailey A, Kastelan M, Legge D et al (2015) Screening for psychological distress in adult primary brain tumor patients and caregivers: considerations for cancer care coordination. Front Oncol 5:1–8
Chambers SK, Girgis A, Occhipinti S, Hutchison S, Turner S, Morris B et al (2012) Psychological distress and unmet supportive care needs in cancer patients and carers who contact cancer helplines. EJCC 21:213–223
Fennell KM, Heckel L, Wilson C, Byrnes M, Livingston PM (2016) How calls from carers, friends and family members of someone affected by cancer differ from those made by people diagnosed with cancer; analysis of four years of South Australian Cancer Council Helpline data. Support Care Cancer 24:2611–2618. https://doi.org/10.1007/s00520-015-3069-y
Groepper S, van der Meer E, Landes T, Bucher H, Stickel A, Goerling U (2016) Assessing cancer-related distress in cancer patients and caregivers receiving outpatient psycho-oncological counselling. Support Care Cancer 24:2351–2357
Sklenarova H, Kruempelmann A, Haun MW, Friedrich H-C, Huber J, Thomas M et al (2015) When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer 121:1513–1519
Vanderwerker LC, Laff RE, Kadan-Lottick NS, McColl S, Prigerson HG (2005) Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. J Clin Oncol 23:6899–6907
Mosher CE, Champion VL, Hanna N, Jalal SI, Fakiris AJ, Birdas TJ et al (2013) Support service use and interest in support services among distress family caregivers of lung cancer patients. Psycho-Oncology 11:1549–1556
Morra M, Thomsen C, Vezina A, Akkerman D, Bright MA, Dickens C et al (2007) The international cancer information service: a worldwide resource. J Cancer Educ 22(Suppl):S61–S69
Boltong A, Ledwick M, Babb K, Sutton C, Ugalde A (2017) Exploring the rationale, experience and impact of using Cancer Information and Support (CIS) services: an international qualitative study. Support Care Cancer 25:1221–1228
Chambers SK, Girgis A, Occhipinti S, Hutchison S, Turner J, McDowell M, Mihalopoulos C, Carter R, Dunn JC (2014) A randomized trial comparing two low-intensity psychological interventions for distressed patients with cancer and their caregivers. Oncol Nurs Forum 41:E256–E266
Hutchison SD, Sargeant H, Morris BA, Hawkes AL, Clutton S, Chambers SK (2011) A community-based approach to cancer counselling for patients and carers: a preliminary study. Psycho-Oncology 20:897–901
Linehan K, Fennell KM, Hughes DL, Wilson CJ (2017) The impact of a telephone-based cancer information and support service on callers’ levels of distress and the acceptability and validity of the Distress Thermometer in the cancer helpline context. Eur J Oncol Nurs 26:49–55. https://doi.org/10.1016/j.ejon.2016.12.005
Livingston PM, White VM, Hayman J, Maunsell E, Dunn SM, Hill D (2010) The psychological impact of a specialist referral and telephone intervention on male cancer patients: a randomised controlled trial. Psycho-Oncology 19:617–625
Cancer Council Australia (2018) What we do. https://www.cancer.org.au/about-us/what-we-do.html
Boltong A, Byrnes M, McKiernan S, Quin N, Chapman K (2015) Exploring the preferences, perceptions and satisfaction of people seeking cancer information and support: implications for the Cancer Council Helpline. AJCN 16:20–28
Livingston P, White V, Hayman J, Hill D (2006) How acceptable is a referral and telephone-based outcall programme for men diagnosed with cancer? A feasibility study. EJCC 15:467–475
Livingston PM, Osborne R, Botti M, Mihalopoulus C, McGuigan S, Heckel L et al (2014) Efficacy and cost-effectiveness of an outcall program to reduce caregiver burden and depression among caregivers of cancer patients [PROTECT]: rationale and design of a randomized controlled trial. BMC Health Serv Res 14:1–8
Heckel L, Fennell KM, Reynolds J, Boltong A, Botti M, Osborne RH, Mihalopoulos C, Chirgwin J, Williams M, Gaskin CJ, Ashley DM, Livingston PM (2018) Efficacy of a telephone outcall program to reduce caregiver burden among caregivers of cancer patients [PROTECT]: a randomised controlled trial. BMC Cancer 18:59. https://doi.org/10.1186/s12885-017-3961-6
Girgis A, Lambert S, Lecathelinais C (2011) The supportive care needs survey for partners and caregivers of cancer survivors: development and psychometric evaluation. Psycho-Oncology 20:387–393
Akizuki N, Akechi T, Nakanishi T, Yoshikawa E, Okamura M, Nakano T, Murakami Y, Uchitomi Y (2003) Development of a brief screening interview for adjustment disorders and major depression in patients with cancer. Cancer 97:2605–2613
Feiten S, Friesenhahn V, Heymanns J, Kleboth K, Koeppler H, Mergenthaler U et al (2013) Psychosocial distress in caregivers of patients with a metastatic solid tumor in routine care: a survey in a community based oncology group practice in Germany. CCO 2:1–10
Hawkes AL, Hughes KL, Hutchison SD, Chambers SK (2010) Feasibility of brief psychological distress screening by a community-based telephone helpline for cancer patients and carers. BMC Cancer 10:14
Australian Institute of Health and Welfare (2004) Rural, regional and remote health: a guide to remoteness classifications. Rural Health Series, AIHW, Canberra
Psycho-oncology Cooperative Research Group (PCRG) (2012) ARIA lookup tool user guide. School of Psychology, The University of Sydney, Sydney
Cancer Council NSW (2006) The Cancer Council NSW annual report. Cancer Council New South Wales, Sydney
Jefford M, Black C, Grogan S, Yeoman G, White V, Akkerman D (2005) Information and support needs of callers to the Cancer Helpline, The Cancer Council Victoria. Eur J Cancer Care 14:113–123
Queensland Cancer Fund (2004) Queensland cancer fund cancer helpline. Quality assurance survey. Queensland Cancer Fund, Brisbane
Mahalik JR, Locke BD, Ludlow LH, Diemer MA, Scott RP, Gottfried M et al (2003) Development of the conformity to masculine norms inventory. Psychol Men Masc 4:3–25
Smith JA, Braunack-Mayer A, Wittert G (2006) What do we know about men’s help-seeking and health service use? MJA 184:81–83
Caasi Macaraeg J, Türk Smith S (2013) Psychological distress and help-seeking attitudes of cancer caregivers on Guam. Pacific Asia Inquiry 4:121–135
Kim Y, Baker F, Spillers RL, Wellisch DK (2006) Psychological adjustment of cancer caregivers with multiple roles. Psycho-Oncology 15:795–804
Acknowledgements
We would like to acknowledge the effort of 13 11 20 nurses at Cancer Council South Australia and Cancer Council Victoria who delivered the outcall program to our study participants and of personnel involved in the recruitment of eligible dyads (Pam Adelson, Kath Colvin, and Stephanie Cowdery).
Funding
This study has been funded by the National Health and Medical Research Council (ID: GNT1044400 RM24525).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and informed consent
The study was in accordance with the Declaration of Helsinki. Ethics approval was obtained from the Deakin University Human Research Ethics Committee (2012–083), the participating health services, and Cancer Councils. Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Online Resource 1
Helpline Nurse Intervention Checklist (PDF 52kb)
Rights and permissions
About this article
Cite this article
Heckel, L., Fennell, K.M., Orellana, L. et al. A telephone outcall program to support caregivers of people diagnosed with cancer: utility, changes in levels of distress, and unmet needs. Support Care Cancer 26, 3789–3799 (2018). https://doi.org/10.1007/s00520-018-4246-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4246-6