Abstract
Objectives
The study aimed to analyze the association between hypertension control and subclinical cerebrovascular health using a comprehensive multimodal imaging approach.
Methods
The study included 200 hypertensive older males without previous cardiovascular diseases. Clinic blood pressure (BP) was measured using a standard approach. Cerebrovascular health was evaluated using magnetic resonance imaging in the following four aspects: Intracranial atherosclerosis as determined by vessel wall imaging; Vascular rarefaction (defined as less discernible vessels on angiography) was evaluated using a custom-developed technique. Cerebral blood flow (CBF) and white matter hyperintensity (WMH) were assessed using arterial spin-labeling imaging and fluid-attenuated inversion recovery imaging, respectively.
Results
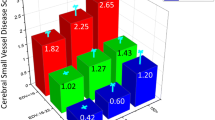
A total of 189 subjects had MRI scans. The mean age was 64.9 (± 7.2) years. For intracranial atherosclerosis, there was a significant association between uncontrolled hypertension and presence of intracranial plaque. When systolic and diastolic BP were analyzed separately, the association remained significant for both. For vascular rarefaction, uncontrolled hypertension was associated with less discernible vessel branches or shorter vessel length on angiography. Further analysis revealed that this is due to uncontrolled diastolic BP, but not uncontrolled systolic BP. There was an association between uncontrolled hypertension and reduced CBF, which was also mainly driven by uncontrolled diastolic BP. We also found that uncontrolled diastolic BP, but not uncontrolled systolic BP, was associated with increased WMH volume.
Conclusions
Uncontrolled hypertension was associated with subclinical cerebrovascular injury globally, with both small and medium-to-large arteries being affected.
Key Points
• In this study, we leveraged the advantage of a series of cutting-edge MR imaging and analysis techniques and found uncontrolled hypertension is associated with subclinical globally compromised cerebrovascular health.
• The detrimental consequences of uncontrolled BP affect not only the small vessels but also the medium-to-large arteries, and uncontrolled systolic and diastolic BP are both independently associated with certain types of cerebrovascular injury.
• Our data suggest that cerebrovascular health is impaired globally in uncontrolled hypertension before the onset of stroke.

Similar content being viewed by others
Abbreviations
- CBF:
-
Cerebral blood flow
- eGFR:
-
Estimated glomerular filtration rate
- UDBP:
-
Uncontrolled diastolic BP
- UH:
-
Uncontrolled hypertension
- USBP:
-
Uncontrolled systolic BP
- WMH:
-
White matter hyperintensities
References
United Nations DoE, Social Affairs PD (2019) World Population Prospects 2019: Highlights
Sheng CS, Liu M, Kang YY et al (2013) Prevalence, awareness, treatment and control of hypertension in elderly Chinese. Hypertens Res 36:824–828
Yoon SS, Carroll MD, Fryar CD (2015) Hypertension prevalence and control among adults: United States, 2011-2014. NCHS Data Brief 1–8
SPRINT MIND Investigators for the SPRINT Research Group, Williamson JD, Pajewski NM et al (2019) Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA 321:553–561
Lane CA, Barnes J, Nicholas JM et al (2019) Associations between blood pressure across adulthood and late-life brain structure and pathology in the neuroscience substudy of the 1946 British birth cohort (Insight 46): an epidemiological study. Lancet Neurol 18:942–952
Muller M, Sigurdsson S, Kjartansson O et al (2014) Joint effect of mid- and late-life blood pressure on the brain: the AGES-Reykjavik study. Neurology 82:2187–2195
Klarenbeek P, van Oostenbrugge RJ, Rouhl RP, Knottnerus IL, Staals J (2013) Higher ambulatory blood pressure relates to new cerebral microbleeds: 2-year follow-up study in lacunar stroke patients. Stroke 44:978–983
Liu LS, Writing Group of Chinese Guidelines for the Management of Hypertension (2011) 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi 39:579–615
Joint Committee for Guideline Revision (2019) 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the Revision Committee of Chinese Guidelines for prevention and treatment of hypertension. J Geriatr Cardiol 16:182–241
Guo X, Pantoni L, Simoni M et al (2009) Blood pressure components and changes in relation to white matter lesions: a 32-year prospective population study. Hypertension 54:57–62
Miura K, Soyama Y, Morikawa Y et al (2004) Comparison of four blood pressure indexes for the prediction of 10-year stroke risk in middle-aged and older Asians. Hypertension 44:715–720
Chen L, Mossa-Basha M, Balu N et al (2018) Development of a quantitative intracranial vascular features extraction tool on 3D MRA using semiautomated open-curve active contour vessel tracing. Magn Reson Med 79:3229–3238
Chen L, Mossa-Basha M, Sun J et al (2019) Quantification of morphometry and intensity features of intracranial arteries from 3D TOF MRA using the intracranial artery feature extraction (iCafe): a reproducibility study. Magn Reson Imaging 57:293–302
Chen L, Sun J, Hippe DS et al (2019) Quantitative assessment of the intracranial vasculature in an older adult population using iCafe. Neurobiol Aging 79:59–65
Alsop DC, Detre JA, Golay X et al (2015) Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: a consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med 73:102–116
Roura E, Oliver A, Cabezas M et al (2015) A toolbox for multiple sclerosis lesion segmentation. Neuroradiology 57:1031–1043
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Fukuhara M, Arima H, Ninomiya T et al (2013) White-coat and masked hypertension are associated with carotid atherosclerosis in a general population: the Hisayama study. Stroke 44:1512–1517
Cardoso CR, Marques CE, Leite NC, Salles GF (2012) Factors associated with carotid intima-media thickness and carotid plaques in type 2 diabetic patients. J Hypertens 30:940–947
Prati P, Vanuzzo D, Casaroli M et al (2006) Determinants of carotid plaque occurrence. A long-term prospective population study: the San Daniele Project. Cerebrovasc Dis 22:416–422
Alexander MD, Yuan C, Rutman A et al (2016) High-resolution intracranial vessel wall imaging: imaging beyond the lumen. J Neurol Neurosurg Psychiatry 87:589–597
Riddle DR, Sonntag WE, Lichtenwalner RJ (2003) Microvascular plasticity in aging. Ageing Res Rev 2:149–168
Antonios TF, Singer DR, Markandu ND, Mortimer PS, MacGregor GA (1999) Structural skin capillary rarefaction in essential hypertension. Hypertension 33:998–1001
Vernooij MW, van der Lugt A, Ikram MA et al (2008) Total cerebral blood flow and total brain perfusion in the general population: the Rotterdam Scan Study. J Cereb Blood Flow Metab 28:412–419
Dai W, Lopez OL, Carmichael OT, Becker JT, Kuller LH, Gach HM (2008) Abnormal regional cerebral blood flow in cognitively normal elderly subjects with hypertension. Stroke 39:349–354
Beason-Held LL, Moghekar A, Zonderman AB, Kraut MA, Resnick SM (2007) Longitudinal changes in cerebral blood flow in the older hypertensive brain. Stroke 38:1766–1773
Tryambake D, He J, Firbank MJ, O'Brien JT, Blamire AM, Ford GA (2013) Intensive blood pressure lowering increases cerebral blood flow in older subjects with hypertension. Hypertension 61:1309–1315
Faraci FM, Heistad DD (1990) Regulation of large cerebral arteries and cerebral microvascular pressure. Circ Res 66:8–17
Marcus J, Gardener H, Rundek T et al (2011) Baseline and longitudinal increases in diastolic blood pressure are associated with greater white matter hyperintensity volume: the northern Manhattan study. Stroke 42:2639–2641
SPRINT MIND Investigators for the SPRINT Research Group, Nasrallah IM, Pajewski NM et al (2019) Association of intensive vs standard blood pressure control with cerebral white matter lesions. JAMA 322:524–534
Dufouil C, de Kersaint-Gilly A, Besancon V et al (2001) Longitudinal study of blood pressure and white matter hyperintensities: the EVA MRI Cohort. Neurology 56:921–926
Lamar M, Wu D, Durazo-Arvizu RA et al (2017) Cognitive associates of current and more intensive control of hypertension: findings from the Hispanic Community Health Study/Study of Latinos. Am J Hypertens 30:624–631
Saxby BK, Harrington F, Wesnes KA, McKeith IG, Ford GA (2008) Candesartan and cognitive decline in older patients with hypertension: a substudy of the SCOPE trial. Neurology 70:1858–1866
Acknowledgments
We would like to thank all the participants of the BRAVE-1 study.
Funding
The study is supported by a grant from Jiangsu Science and Technology Department (BE2017762) to Dr. Junwei Yang.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Junwei Yang
Conflict of interest
The authors of this manuscript declare relationships with the following companies: Dr. Wenjin Liu is supported by NVIDIA Corporation with the donation of the Titan V GPU used for this research.
Statistics and biometry
One of the authors (Dr. Wenjin Liu) has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Methodology
• cross-sectional study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Liu, W., Huang, X., Liu, X. et al. Uncontrolled hypertension associates with subclinical cerebrovascular health globally: a multimodal imaging study. Eur Radiol 31, 2233–2241 (2021). https://doi.org/10.1007/s00330-020-07218-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07218-5