Abstract
Summary
The mechanisms through which excessive sitting time impacts health are important to understand. This study found that each hour of sitting per day was not associated with physical function, although associations with poor body composition were observed. Reducing sitting time for improved weight management in older adults needs further exploration.
Introduction
To examine the association of sitting time and breaks in sitting time with muscle mass, strength, function, and inflammation in older Australians.
Methods
Data from the thigh-worn activPAL3™ monitor (7-day continuous wear) was used to derive time spent sitting (hours) and total number of sit-stand transitions per day. Body composition (dual energy X-ray absorptiometry), lower-body muscle strength, function (timed up-and-go [TUG], 4-m gait speed, four square step test, 30-second sit-to-stand), and serum inflammatory markers (interleukin-[IL-6], IL-8, IL-10, tumor necrosis factor-alpha [TNF-α], and adiponectin) were measured. Multiple regression analyses, adjusted for age, sex, ethnicity, education, employment status, marital status, number of prescription medications, smoking status, vitamin D, and stepping time, were used to assess the associations.
Results
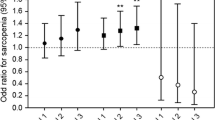
Data from 123 community-dwelling older adults (aged 65–84 years, 63% female) were used. Total daily sitting time was associated with lower percentage lean mass (β [95%CI], − 1.70% [− 2.30, − 1.10]) and higher total body fat mass (2.92 kg [1.94, 3.30]). More frequent breaks in sitting time were associated with a 45% reduced risk of having pre-sarcopenia (OR = 0.55; 95% CI 0.34, 0.91; model 1), defined as appendicular lean mass divided by BMI. No significant associations were observed for sitting time or breaks in sitting with measures of muscle strength, function, or inflammation.
Conclusion
In older community-dwelling adults, greater sitting time was associated with a lower percentage lean mass, while more frequent breaks in sitting time were associated with lower odds of having pre-sarcopenia. This suggests that reducing sedentary time and introducing frequent breaks in sedentary time may be beneficial for improving body composition in healthy older adults.
Similar content being viewed by others
References
Roubenoff R (2004) Sarcopenic obesity: the confluence of two epidemics. Obes Res 12:887–888
Tarantino U, Baldi J, Celi M, Rao C, Liuni FM, Iundusi R, Gasbarra E (2013) Osteoporosis and sarcopenia: the connections. Aging Clin Exp Res 25(Suppl 1):S93–S95
Landi F, Liperoti R, Russo A, Giovannini S, Tosato M, Capoluongo E, Bernabei R, Onder G (2012) Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr 31:652–658
Landi F, Cruz-Jentoft AJ, Liperoti R, Russo A, Giovannini S, Tosato M, Capoluongo E, Bernabei R, Onder G (2013) Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from ilSIRENTE study. Age Ageing 42:203–209
Landi F, Calvani R, Ortolani E, Salini S, Martone AM, Santoro L, Santoliquido A, Sisto A, Picca A, Marzetti E (2017) The association between sarcopenia and functional outcomes among older patients with hip fracture undergoing in-hospital rehabilitation. Osteoporos Int 28:1569–1576
Phillips A, Strobl R, Vogt S, Ladwig KH, Thorand B, Grill E (2017) Sarcopenia is associated with disability status-results from the KORA-Age study. Osteoporos Int 28:2069–2079
Paterson DH, Warburton DER (2010) Physical activity and functional limitations in older adults: a systematic review related to Canada’s Physical Activity Guidelines. Int J Behav Nutr Phys Act 7:38–60
Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, Cumming RG, Herbert RD, Close JC, Lord SR (2016) Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med
Bennie JA, Pedisic Z, van Uffelen JG, Charity MJ, Harvey JT, Banting LK, Vergeer I, Biddle SJ, Eime RM (2016) Pumping iron in Australia: prevalence, trends and sociodemographic correlates of muscle strengthening activity participation from a national sample of 195,926 adults. PLoS One 11:e0153225
Harvey JA, Chastin SF, Skelton DA (2014) How sedentary are older people? A systematic review of the amount of sedentary behavior. J Aging Phys Act 23:471–487
de Rezende LF, Rodrigues Lopes M, Rey-Lopez JP, Matsudo VK, Luiz Odo C (2014) Sedentary behavior and health outcomes: an overview of systematic reviews. PLoS One 9:e105620
Sedentary Behaviour Research Network (2012) Standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab 37:540–542
Keevil VL, Cooper AJ, Wijndaele K, Luben R, Wareham NJ, Brage S, Khaw KT (2016) Objective sedentary time, moderate-to-vigorous physical activity, and physical capability in a British cohort. Med Sci Sports Exerc 48:421–429
Chastin SF, Ferriolli E, Stephens NA, Fearon K, Greig C (2012) Relationship between sedentary behaviour, physical activity, muscle quality and body composition in healthy older adults. Age Ageing 41:111–114
Gianoudis J, Bailey CA, Daly RM (2014) Associations between sedentary behaviour and body composition, muscle function and sarcopenia in community-dwelling older adults. Osteoporos Int 26:571–579
Sardinha LB, Santos DA, Silva AM, Baptista F, Owen N (2015) Breaking-up sedentary time is associated with physical function in older adults. J Gerontol A Biol Sci Med Sci 70:119–124
Henson J, Yates T, Edwardson CL, Khunti K, Talbot D, Gray LJ, Leigh TM, Carter P, Davies MJ (2013) Sedentary time and markers of chronic low-grade inflammation in a high risk population. PLoS One 8:e78350
Brinkley TE, Leng X, Miller ME, Kitzman DW, Pahor M, Berry MJ, Marsh AP, Kritchevsky SB, Nicklas BJ (2009) Chronic inflammation is associated with low physical function in older adults across multiple comorbidities. J Gerontol A Biol Sci Med Sci 64:455–461
Beyer I, Mets T, Bautmans I (2012) Chronic low-grade inflammation and age-related sarcopenia. Curr Opin Clin Nutr Metab Care 15:12–22
Daly RM, Gianoudis J, Prosser M, Kidgell D, Ellis KA, O'Connell S, Nowson CA (2015) The effects of a protein enriched diet with lean red meat combined with a multi-modal exercise program on muscle and cognitive health and function in older adults: study protocol for a randomised controlled trial. Trials 16:339
Brink TL, Yesavage JA, Lum O, Heersema PH, Adey M, Rose TL (1982) Screening tests for geriatric depression. Clin Gerontol 1:37–43
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23:433–441
Grant PM, Ryan CG, Tigbe WW, Granat MH (2006) The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med 40:992–997
Grant PM, Dall PM, Mitchell SL, Granat MH (2008) Activity-monitor accuracy in measuring step number and cadence in community-dwelling older adults. J Aging Phys Act 16:201–214
Reid N, Daly RM, Winkler EA, Gardiner PA, Eakin EG, Owen N, Dunstan DW, Healy GN (2016) Associations of monitor-assessed activity with performance-based physical function. PLoS One 11:e0153398
Willet WC, Howe GR, Kushi LH (1997) Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr 65:1220S–1228S
Bohannon RW (2001) Measuring knee extensor muscle strength. Am J Phys Med Rehabil 80:13–18
Daly RM, Duckham RL, Tait JL, Rantalainen T, Nowson CA, Taaffe DR, Sanders K, Hill KD, Kidgell DJ, Busija L (2015) Effectiveness of dual-task functional power training for preventing falls in older people: study protocol for a cluster randomised controlled trial. Trials 16:120
Dite W, Temple VA (2002) A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil 83:1566–1571
Jones CJ, Rikli RE, Beam WC (1999) A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport 70:113–119
Hofheinz M, Mibs M (2016) The prognostic validity of the timed up and go test with a dual task for predicting the risk of falls in the elderly. Gerontol Geriatr Med 2:1–5
Kim HJ, Park I, Lee HJ, Lee O (2016) The reliability and validity of gait speed with different walking pace and distances against general health, physical function, and chronic disease in aged adults. J Exerc Nutrition Biochem 20:46–50
Dawson-Hughes B, Bischoff-Ferrari H (2016) Considerations concerning the definition of sarcopenia. Osteoporos Int 27:3139–3144
Cruz-Jentoft AJ, Schneider SM, Topinková E et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing 39:412–423
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, Ferrucci L, Guralnik JM, Fragala MS, Kenny AM, Kiel DP, Kritchevsky SB, Shardell MD, Dam TTL, Vassileva MT (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 69:547–558
Department of Health Web site (2013) Recommendations on physical activity for health for older Australians. Australian Government. http://www.health.gov.au
Smith L, Thomas EL, Bell JD, Hamer M (2014) The association between objectively measured sitting and standing with body composition: a pilot study using MRI. BMJ Open 4:e005476
Santos DA, Silva AM, Baptista F, Santos R, Vale S, Mota J, Sardinha LB (2012) Sedentary behavior and physical activity are independently related to functional fitness in older adults. Exp Gerontol 47:908–912
Gennuso KP, Gangnon RE, Matthews CE, Thraen-Borowski KM, Colbert LH (2013) Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc 45:1493–1500
Seguin R, Lamonte M, Tinker L, Liu J, Woods N, Michael YL, Bushnell C, Lacroix AZ (2012) Sedentary behavior and physical function decline in older women: findings from the Women’s Health Initiative. J Aging Res 2012:10
Rosenberg DE, Bellettiere J, Gardiner PA, Villarreal VN, Crist K, Kerr J (2016) Independent associations between sedentary behaviors and mental, cognitive, physical, and functional health among older adults in retirement communities. J Gerontol A Biol Sci Med Sci 71:78–83
Healy GN, Clark BK, Winkler EAH, Gardiner PA, Brown WJ, Matthews CE (2011) Measurement of adults’ sedentary time in population-based studies. Am J Prev Med 41:216–227
Wullems JA, Verschueren SM, Degens H, Morse CI, Onambele GL (2016) A review of the assessment and prevalence of sedentarism in older adults, its physiology/health impact and non-exercise mobility counter-measures. Biogerontology 17:547–565
Rikli RE, Jones CJ (1999) Functional fitness normative scores for community-residing older adults, ages 60-94. J Aging Phys Act 7:162–181
Monteiro R, Azevedo I (2010) Chronic inflammation in obesity and the metabolic syndrome. Mediat Inflamm 2010:10
Aggio DA, Sartini C, Papacosta O, Lennon LT, Ash S, Whincup PH, Wannamethee SG, Jefferis BJ (2016) Cross-sectional associations of objectively measured physical activity and sedentary time with sarcopenia and sarcopenic obesity in older men. Prev Med 91:264–272
Yu S, Appleton S, Adams R, Chapman I, Wittert G, Visvanathan T, Visvanathan R (2014) The impact of low muscle mass definition on the prevalence of sarcopenia in older Australians. Biomed Res Int 2014:361790
Judice PB, Santos DA, Hamilton MT, Sardinha LB, Silva AM (2015) Validity of GT3X and Actiheart to estimate sedentary time and breaks using ActivPAL as the reference in free-living conditions. Gait Posture 41:917–922
Aadland E, Ylvisaker E (2015) Reliability of objectively measured sedentary time and physical activity in adults. PLoS One 10:e0133296
Acknowledgements
This work was supported by the National Health and Medical Research Council of Australia (Centre of Research Excellence Grant #1057608 to G.N.H., and E.G.E., with a top-up scholarship provided to N.R.; Senior Research Fellowship #511001 to E.G.E.; Career Development Fellowship #108029 to G.N.H), the National Health and Medical Research Council of Australia and Australian Research Council (Dementia Research Development Fellowship #110331 to P.A.G.), and the Australian Federal Government (Australian Postgraduate Award Scholarship to N.R.). This study was part of a larger intervention trial that was supported by a competitive peer-reviewed grant from Meat and Livestock Australia (D.MHN.0303).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
ESM 1
(DOCX 15 kb).
Rights and permissions
About this article
Cite this article
Reid, N., Healy, G.N., Gianoudis, J. et al. Association of sitting time and breaks in sitting with muscle mass, strength, function, and inflammation in community-dwelling older adults. Osteoporos Int 29, 1341–1350 (2018). https://doi.org/10.1007/s00198-018-4428-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4428-6