Abstract
Purpose
As global initiatives increase patient access to surgical treatments, there is a need to define optimal levels of perioperative care. Our aim was to describe the relationship between the provision and use of critical care resources and postoperative mortality.
Methods
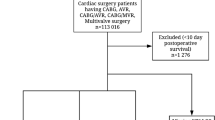
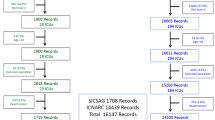
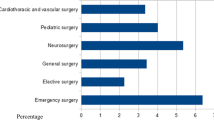
Planned analysis of data collected during an international 7-day cohort study of adults undergoing elective in-patient surgery. We used risk-adjusted mixed-effects logistic regression models to evaluate the association between admission to critical care immediately after surgery and in-hospital mortality. We evaluated hospital-level associations between mortality and critical care admission immediately after surgery, critical care admission to treat life-threatening complications, and hospital provision of critical care beds. We evaluated the effect of national income using interaction tests.
Results
44,814 patients from 474 hospitals in 27 countries were available for analysis. Death was more frequent amongst patients admitted directly to critical care after surgery (critical care: 103/4317 patients [2%], standard ward: 99/39,566 patients [0.3%]; adjusted OR 3.01 [2.10–5.21]; p < 0.001). This association may differ with national income (high income countries OR 2.50 vs. low and middle income countries OR 4.68; p = 0.07). At hospital level, there was no association between mortality and critical care admission directly after surgery (p = 0.26), critical care admission to treat complications (p = 0.33), or provision of critical care beds (p = 0.70). Findings of the hospital-level analyses were not affected by national income status. A sensitivity analysis including only high-risk patients yielded similar findings.
Conclusions
We did not identify any survival benefit from critical care admission following surgery.



Similar content being viewed by others
References
The Lancet commission on global surgery (2016) http://www.lancetglobalsurgery.org/. Accessed 3 Nov 2016
Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, Gawande AA (2008) An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 372:139–144
Weiser TG, Haynes AB, Molina G, Lipsitz SR, Esquivel M, Uribe-Leitz T, Fu R, Azad T, Chao TE, Berry WR, Gawande AA (2015) Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. Lancet 385(Suppl 2):S11
Alkire BC, Raykar NP, Shrime MG, Weiser TG, Bickler SW, Rose JA, Nutt CT, Greenberg SL, Kotagal M, Riesel JN, Esquivel M, Uribe-Leitz T, Molina G, Roy N, Meara JG, Farmer PE (2015) Global access to surgical care: a modelling study. Lancet Glob Health 3:e316–323
Rose J, Weiser TG, Hider P, Wilson L, Gruen RL, Bickler SW (2015) Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health 3:S13–20
Ghaferi AA, Birkmeyer JD, Dimick JB (2009) Variation in hospital mortality associated with inpatient surgery. New Engl J Med 361:1368–1375
Khuri SF, Daley J, Henderson W, Hur K, Demakis J, Aust JB, Chong V, Fabri PJ, Gibbs JO, Grover F, Hammermeister K, Irvin G 3rd, McDonald G, Passaro E Jr, Phillips L, Scamman F, Spencer J, Stremple JF (1998) The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 228:491–507
Pearse RM, Harrison DA, James P, Watson D, Hinds C, Rhodes A, Grounds RM, Bennett ED (2006) Identification and characterisation of the high-risk surgical population in the United Kingdom. Crit Care 10:R81
Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, Vallet B, Vincent JL, Hoeft A, Rhodes A, European Surgical Outcomes Study group for the trials groups of the European Society of Intensive Care Medicine and the European Society of Anaesthesiology (2012) Mortality after surgery in Europe: a 7 day cohort study. Lancet 380:1059–1065
Gillies MA (2016) Intensive care utilisation and outcomes after high-risk surgery in Scotland: a population based cohort study. Brit J Anaesth. doi:10.1093/bja/aew396
Findlay G, Goodwin A, Protopappa K, Smith N, Mason M (2011) Knowing the risk: a review of the peri-operative care of surgical patients. National Confidential Enquiry into Patient Outcome and Death, London
Jhanji S, Thomas B, Ely A, Watson D, Hinds CJ, Pearse RM (2008) Mortality and utilisation of critical care resources amongst high-risk surgical patients in a large NHS trust. Anaesthesia 63:695–700
Glance LG, Lustik SJ, Hannan EL, Osler TM, Mukamel DB, Qian F, Dick AW (2012) The surgical mortality probability model: derivation and validation of a simple risk prediction rule for noncardiac surgery. Ann Surg 255:696–702
Jencks SF, Williams MV, Coleman EA (2009) Rehospitalizations among patients in the Medicare fee-for-service program. New Engl J Med 360:1418–1428
Noordzij PG, Poldermans D, Schouten O, Bax JJ, Schreiner FA, Boersma E (2010) Postoperative mortality in the Netherlands: a population-based analysis of surgery-specific risk in adults. Anesthesiology 112:1105–1115
Yu PC, Calderaro D, Gualandro DM, Marques AC, Pastana AF, Prandini JC, Caramelli B (2010) Non-cardiac surgery in developing countries: epidemiological aspects and economical opportunities—the case of Brazil. PLoS One 5:e10607
Pearse RM, Holt PJ, Grocott MP (2011) Managing perioperative risk in patients undergoing elective non-cardiac surgery. BMJ 343:d5759
Gillies MA, Power GS, Harrison DA, Fleming A, Cook B, Walsh TS, Pearse RM, Rowan KM (2015) Regional variation in critical care provision and outcome after high-risk surgery. Intensive Care Med 41:1809–1816
Ozdemir BA, Sinha S, Karthikesalingam A, Poloniecki JD, Pearse RM, Grocott MP, Thompson MM, Holt PJ (2016) Mortality of emergency general surgical patients and associations with hospital structures and processes. Br J Anaesth 116:54–62
Wunsch H, Gershengorn HB, Cooke CR, Guerra C, Angus DC, Rowe JW, Li G (2016) Use of intensive care services for medicare beneficiaries undergoing major surgical procedures. Anesthesiology 124(4):899–907
Gillies MA, Pearse RM (2016) Intensive care after high-risk surgery: what’s in a name? Anesthesiology 124(4):761–762
International Surgical Outcomes Study Group (2016) Global patient outcomes after elective surgery: prospective cohort study in 27 low, middle and high income countries. Br J Anaesth 117(5):601–609
Jammer I, Wickboldt N, Sander M, Smith A, Schultz MJ, Pelosi P, Leva B, Rhodes A, Hoeft A, Walder B, Chew MS, Pearse RM (2015) Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol 32(2):88–105
Rabe-Hesketh S, Skrondal A (2012) Multilevel and longitudinal modeling using stata. Stata, Texas
Harrell FE (2001) Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Springer, New York
World Bank (2016) Classification of national income. http://www.worldbank.org/en/country. Accessed 3 Nov 2016
James S, Jhanji S, Smith A, O’Brien G, Fitzgibbon M, Pearse RM (2014) Comparison of the prognostic accuracy of scoring systems, cardiopulmonary exercise testing, and plasma biomarkers: a single-centre observational pilot study. Br J Anaesth 112:491–497
Griffiths P, Ball J, Drennan J, James L, Jones J, Recio-Saucedo A, Simon M (2014) The association between patient safety outcomes and nurse/healthcare assistant skill mix and staffing levels and factors that may influence staffing requirements. National Institute for Health and Care Excellence, London
Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH (2003) Educational levels of hospital nurses and surgical patient mortality. JAMA 290:1617–1623
Blegen MA, Goode CJ, Spetz J, Vaughn T, Park SH (2011) Nurse staffing effects on patient outcomes: safety-net and non-safety-net hospitals. Med Care 49:406–414
Cho SH, Ketefian S, Barkauskas VH, Smith DG (2003) The effects of nurse staffing on adverse events, morbidity, mortality, and medical costs. Nurs Res 52:71–79
McGillis Hall L, Doran D, Pink GH (2004) Nurse staffing models, nursing hours, and patient safety outcomes. J Nurs Adm 34:41–45
Silber JH, Rosenbaum PR, McHugh MD, Ludwig JM, Smith HL, Niknam BA, Even-Shoshan O, Fleisher LA, Kelz RR, Aiken LH (2016) Comparison of the value of nursing work environments in hospitals across different levels of patient risk. JAMA Surg 151:527–536
Acknowledgements
This was an investigator initiated study funded by Nestle Health Sciences through an unrestricted research grant, and by a National Institute for Health Research (UK) Professorship held by RP. The study was sponsored by Queen Mary University of London. ISOS investigators were entirely responsible for study design, conduct, and data analysis. The authors had full data access and were solely responsible for data interpretation, drafting and critical revision of the manuscript, and the decision to submit for publication.
Data sharing
The authors are happy to consider data sharing requests from bona fide researchers. Participant consent was not obtained but the presented data are anonymised and risk of identification is low. Enquiries should be addressed to the chief investigator at admin@isos.org.uk.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
RP holds research grants and has given lectures and/or performed consultancy work for Nestle Health Sciences, BBraun, Medtronic, and Edwards Lifesciences, and is a member of the Associate Editorial Board of the British Journal of Anaesthesia. All other authors declare they have no conflicts of interest.
Additional information
Members of study group are listed in the supplementary file.
Take-home message: We analysed data from 44,814 patients in 27 countries to investigate the effect of postoperative critical care on survival. No evidence of survival benefit was found.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kahan, B.C., Koulenti, D., Arvaniti, K. et al. Critical care admission following elective surgery was not associated with survival benefit: prospective analysis of data from 27 countries. Intensive Care Med 43, 971–979 (2017). https://doi.org/10.1007/s00134-016-4633-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4633-8